Virtual doctors are making waves. Atlanta Medical Center (AMC) in Atlanta, Georgia, has closed its doors to two facilities this year, including the most recently closed downtown location. According to Wellstar, the organization that ran these hospitals, the closures are caused by a lack of revenue, a side effect of rising inflation.
Atlanta isn’t the only community affected by this trend. Even rural hospitals have seen an increase in facility closures. Are virtual doctors the solution or the cause?
Read below to find out how virtual doctors are changing healthcare.
Telemedicine exploded during and after the pandemic. A new way to see your doctor on-screen became the norm. And it stuck. Here are a handful of reasons that virtual doctors are now preferred by patients over in-person visits, leaving hospitals and other in-person medical facilities hanging.
Getting into your doctor for a preventative visit or even to solve a new health problem used to take an excessive amount of time.
First, you had to wait on hold to get an appointment, then you had to wait weeks or months for an opening, then you had to commute to the appointment, and when you finally arrived at your scheduled time—you had to wait a little longer until your doctor was ready to see you. That’s a lot of waiting.
Luckily with the recent developments in telemedicine, most of this waiting process has been completely eliminated. No waiting on hold for scheduling, you can get in the same day to see a doctor, and there’s no commute or waiting room to waste your time with.
Telemedicine solves the dilemma of delayed treatment. Telehealth provides an avenue for patients to be seen by doctors and specialists faster than ever before, which means—patients get faster treatment. Today, conditions get treated before they ever have time to fester into major health concerns that require hospitalization.
It’s safe to say that telemedicine cuts down on the need to hospitalize.
Every patient deserves access to medical care. Relying on the outdated infrastructure of brick-and-mortar buildings to meet the entire nation’s medical needs is no longer feasible. Especially when the technology exists to move certain care needs to the digital realm.
Stepping up to the plate, virtual doctors are here to help ease the demand on physical facilities so that they can serve their populations more effectively.
Telemedicine helps by spreading the load of care needs over a larger pool of providers. When a substantial portion of preventative care visits and other types of appointments that don’t require in-person exams can be transitioned online, it makes healthcare more accessible.
Additionally, virtual doctors open doors for access to patients who are affected by hospital or facility closures in their local communities. Physical distance is no longer an obstacle to overcome when it comes to getting medical care for non-emergency situations.
Related: Telemedicine Improves Access to Prenatal Care, But Can We Improve Access to Telemedicine?
When it comes to answering the question posed at the top of this article, the answer is a little bit of both. While telemedicine certainly shifted patients out of hospitals, that’s not a bad thing. Hospitals can now focus on scaling down operations and focusing only on the emergency needs, such as surgical procedures, while leaving preventative and other simple appointments to virtual doctors.
While telemedicine is certainly not the only cause, it has played a part in the shift away from brick-and-mortar facilities. As far as being the solution to hospital closures, virtual doctors certainly proved their value during the pandemic. Telemedicine is here to stay by popular demand and will become the solution for patients who need to see a provider but have no nearby facility available.
Our virtual doctors serve patients in all 50 states. Whether you need to see a primary care physician or a specialist, we’re here to help. Our mission is to provide access to healthcare. If your community recently experienced a shut down of a medical facility or you’ve heard rumblings of disruption, get established with our online doctors today so that you can always get care when the need arises.
Book Appointment Now Call For An Appointment

Imagine a world where you can’t get in to see your doctor for months or even years. Whether you simply need a prescription refill or help diagnosing and managing a chronic medical condition like diabetes, both can produce scary, or even life-threatening, scenarios.
Now, consider that the United States isn’t that far from this reality. In a 2021 report, the Association of American Medical Colleges (AAMC) predicted that a physician shortage is coming to the US. By 2034, the country will fall short of meeting the appropriate physician-to-patient ratios.
In fact, the AAMC believes that the US will fall between 40,000 to 124,000 doctors short in the next decade or so.
It makes sense that densely-populated areas require more doctors in order to meet healthcare needs. That’s where the physician-to-patient ratio comes in. If you can measure this ratio, it tells you whether you have enough doctors to meet a geographical area’s healthcare needs.
Most states within the USA fall below the ideal physician-to-patient ratio. An ideal number is around 270 physicians per 100,000 people. This equates to about 370 patients per doctor. Many states hover around a rate closer to 200:100,000.
The governmental agency known as the Health Resources & Services Administration (HRSA) works to increase healthcare access to vulnerable populations (geographically isolated, economically or medically vulnerable). Reports are available on their website. These reports show where vulnerable populations are located and where physicians are needed the most.
Nevada has been experiencing a physician shortage for some time. Currently, the state’s ratio remains around 200:100,000. Read more here about the OB/GYN Physician Shortage in Las Vegas.
HRSA reports displaying Health Professional Shortage Areas (HPSA) show regions where there is a shortage of providers. Nevada shows 75 areas with a primary care physician shortage, plus numerous dental and mental health areas where there is a shortage of specialists to serve these populations.
A search on medically underserved areas from HRSA shows 25 regions within the state have underserved areas and populations. Specifically, these areas in Las Vegas are underserved:
It is My Virtual Physician’s mission to provide access to healthcare for men, women, and children. That’s why we offer online telemedicine visits for patients in any US state. This helps break down geographical barriers in order to increase the real physician-to-patient ratio. On top of that, we have taken it a step further with our hybrid clinic located in Las Vegas.
Read about our hybrid clinic’s opening here: My Virtual Physician Celebrates Las Vegas Hybrid Clinic Opening.
This clinic helps to serve populations who may not have access to the digital requirements of telemedicine. We provide a private room that our patients can use to meet virtually with our doctors inside the clinic located at 2217 Paradise Road in Las Vegas.
Additionally, the clinic provides immediate access for all populations. Walk-ins are welcome during business hours. Find out more here. Our doctors can provide primary care needs as well as specialty visits. In addition to our primary care doctors, we also have board-certified OBGYNs and Pediatricians ready to meet with patients.

There’s been a recent spike in positive RSV tests in the Las Vegas region. CDC data shows a jump to over 5% of positive PCR tests that began in September and October.
This spike resembles last year’s Vegas RSV data for September, but preliminary information looks like it might be doubling October’s numbers. So is it cause for concern?
Here’s everything you need to know about RSV if you’re living or staying in Las Vegas.
Respiratory syncytial virus (RSV) is a seasonal respiratory virus that resembles the common cold, but can develop into a more serious illness for some people.
Each year, this virus spikes during cold weather months, typically late fall. This cycle, the CDC surveillance noticed that the peak is happening earlier than usual across the country, and hospitals are seeing more patients coming in with RSV.
The symptoms of RSV appear within a week after exposure, and they can include a series of effects lasting one to two weeks, such as:
For infants under one year old, the symptoms can be difficult to identify and can include the following:
For most people, the RSV virus is not dangerous. The immune system naturally takes care of the virus with a one-to-two-week recovery period. Some populations are at a higher risk (babies under the age of one) of developing serious complications, including:
RSV is so common that most children contract and recover from RSV before turning two years old. Having RSV isn’t necessarily a cause for concern—but keep a close eye on the more troubling symptoms involving difficulty breathing and look for signs of dehydration.
Infants, the elderly, and those with compromised immune systems or existing breathing problems are at a higher risk when it comes to RSV. Their bodies may struggle more than others to heal from the virus and may require medical intervention.
Here’s a list of specific factors that may also put you or your loved ones at a higher risk of RSV-related complications:
If you or someone in your family is at a higher risk of complications from RSV, then follow the precautions in the next section to reduce your chances of exposure. If you have a trip planned to Vegas with your infant, you may want to reschedule until your baby is older and the spike in RSV has passed for the season.
Follow these tips to help reduce the spread of RSV in Las Vegas and elsewhere:
If you believe you or your child has RSV, stay home for at least one week after symptoms begin. Schools and daycares tend to spread RSV. People with cold or flu-like symptoms should avoid contact with those who are at a higher risk of complications from RSV until they have recovered.
RSV testing is available. There are several types of tests that can be used to diagnose the viral infection. Testing is recommended for more vulnerable populations with symptoms who are at a higher risk of developing severe respiratory infections from the virus.
The testing process varies but one method is very similar to Covid-19 testing; using a nasal swab. Another method requires flushing the nose with saline liquid to collect the sample for lab testing.
In most cases, RSV clears up on its own, and no medical intervention is required. There are not currently any vaccines or medications that are used for recovering from RSV.
Here are some natural remedies that help to relieve the symptoms:
If you need help treating the symptoms and over-the-counter medications are not helping, or you’re not sure about giving your child cold medicine, contact your doctor or pediatrician.
In rare cases, infants or older adults may require treatment in a hospital setting for a few days so that they can get oxygen or IV fluids to help with breathing and hydration while the body recovers. Out of 100 infants under six months old who test positive for RSV, only one or two will require hospitalization.
RSV is a common virus that comes around every year and doesn’t pose much of a problem for most people. However, for some, it can become life-threatening. If you or someone in your family is at a higher risk for RSV-related complications and you’re concerned, there are steps you can take to minimize your exposure.
If you’re having symptoms and would like to get tested for RSV because you or someone you are around frequently is at a high risk for complications, contact My Virtual Physician to set up RSV testing or get medical advice to treat symptoms.
Book Appointment Now Call For An Appointment

My Virtual Physician has an exciting announcement to celebrate: our hybrid clinic on Paradise Road is now open in Las Vegas!
My Virtual Physician’s mission is to provide safe, secure, and convenient access to healthcare for men, women, and children. In other words, we use telemedicine to fill the healthcare access gap that’s left by the reality that many doctors don’t offer same-day services. Patients who need to see a doctor now have the ability to meet virtually with our team of physicians with same-day appointments.
Our online telemedicine services launched during the pandemic, have grown exponentially, and continue strong today—providing quality healthcare access nationwide, online. We credit our growing team of doctors for our success.
But My Virtual Physician aims higher than simply providing online access to those who have the right equipment for a virtual visit (such as a smartphone or computer equipped with a camera and mic).
Other limitations exist with providing this type of healthcare solely online, including not having a private or safe place to interact virtually and the lack of medical equipment for taking vitals and collecting labs for diagnostics.
To overcome this challenge, My Virtual Physician opened its first one-of-a-kind hybrid clinic in Las Vegas. We’re excited to announce that, despite some major obstacles, we have successfully launched our first physical walk-in location.
Related: Hybrid Medical Clinics: Expanding OBGYN Access in Las Vegas
My Virtual Physician’s hybrid medical clinic is now open at 2217 Paradise Road in Las Vegas. Walk-ins are welcome. Find out our current hours or book an appointment (if preferred) here.
We are pleased to welcome men, women, and children into the physical clinic for a virtual visit in our private patient room, where our videoconferencing equipment is already set up and ready to go. We provide women’s health, pediatric, and primary care services in our hybrid clinic.
My Virtual Physician is proud to have opened the first clinic in Vegas that offers immediate access to online healthcare for those who may not have access to the equipment or private space. We welcome all to come visit us. Find us on Paradise Road! Get Directions Here.
Related: Now Available: Walk-in STD Testing in Las Vegas at Hybrid Clinic
 Inside Our Las Vegas Hybrid Clinic
Inside Our Las Vegas Hybrid ClinicTake a peek inside our clinic, where our certified medical assistant (CMA) will greet you! We have a comfortable waiting room for busier times. We also have a private room for patient use where our CMA will take your vitals, give you the tools to collect samples if needed for labs, and then you can meet virtually with our doctors with our private and secure videoconferencing setup.
At times, we do staff the clinic with a nurse manager and other medical professionals who can provide additional services such as wound care, vaccinations, ultrasounds, and more. If you’re interested in these services, please call ahead to (888) 224-0804 so that we can make sure the appropriate staff is present for your visit.
My Virtual Physician offers affordable and immediate access to patients at our new hybrid clinic in Las Vegas. Click to find out more about which services we offer. Welcome to our clinic!
Did you know that the CDC reports nearly 700 Americans die each summer from extreme heat? Higher outdoor temperatures can lead to hyperthermia (high body temperature), ultimately resulting in complications. It's August, and we are getting closer to fall. However, summer is not over yet.
Prolonged heat exposure in the summer months can cause heat stroke and dehydration. What's more, extreme heat can worsen certain health concerns, including heart problems. Complications and illnesses due to heat are preventable.
Here we explain why high summer temperatures are concerning and what precautions you should take this summer.

Intense heat presents a health risk for everyone, especially those with heart conditions. They face danger and even an increased risk of death. That is because the way that our bodies adjust to heat can cause internal stress and even restrict blood flow. Also, blood pressure can increase when the body tries to cool itself, which strains vessels and the heart.
If you have ever had a stroke or a heart attack, your body may not be strong enough to compensate for the strain caused by extreme heat. If you start to feel sick or extremely uncomfortable from the heat, it could be a sign that something is going on. So, you should take action to calm and cool the body.
Here are a few ways to help your body manage the stress of extreme temperatures this summer.
During the summer, you must stay hydrated. Taking in enough fluids each day is essential to avoiding heat-related complications. Unless your doctor restricts your fluid intake because of heart or kidney disease, you should drink plenty of water. Avoid caffeinated beverages. Also, eat fruits that are high in water content, such as:
Fruits also contain fiber, which can help balance your body's hydration.
Note: If your doctor has limited your water intake, ask how much you should drink this summer.
This summer, avoiding sugary drinks like soda and juices would be best because they may increase the risks of high blood pressure, obesity and diabetes. They can also lead to a "sugar crash," which can drain your energy and harm your teeth.
Salts and other minerals in the body are essential for vital body functions, including:
Heavy sweating during the summer results in loss of electrolytes, like salts and minerals. It is best to replenish electrolytes during this season through a balanced diet. Consider adding a multivitamin to your diet to stay healthy so that you will be able to avoid heat-related health complications this summer.
If you are going to be outside during the summer, experts recommend wearing loose-fitting, lightweight, and light-colored clothes. Light color clothes absorb less heat and may reflect the sun's rays compared to dark colors and heavy clothes.
In extreme heat, it is best to stay indoors in air-conditioned places. If you do not have air-conditioning at home, you could go to a public place like the library. Resting in air-conditioned buildings for part of the day will cool your body. Remember that fans can make you comfortable but may not prevent heat-related complications when the temperature is very high.
If you don't have adequate air conditioning, you can also try to take a cool bath or shower.
Avoid using your stove and oven as much as possible to keep your home cool.
If you must be outside, try to schedule outdoor activities during the coolest times of day, morning and evening hours. Rest in shady areas.
It is important to use sunblock because sunburn reduces your body's ability to cool down. It also makes you vulnerable to dehydration.
You may be able to prevent sunburn by wearing hats, sunglasses, and a broad-spectrum sunscreen outdoors. Try to apply SPF 15 or higher sunscreen 30 minutes before going outdoors.
Although anyone can suffer from heat-related complications, some people are at higher risk. These may include:
If you have loved ones at risk this summer, visit them or check on them frequently, especially during the day. Children and older adults may need extra help during summer.
Also, watch local news updates on extreme temperatures and safety precautions.
If you or someone you know is not tolerating extreme heat this summer, here are some of the signs and symptoms you might notice.
If you are with someone who complains of these heat-related symptoms, help them find a place to rest and cool off with a fan and a cold towel. Call a healthcare provider if the symptoms do not improve.
Talk with one of our expert doctors if you want to learn more about virtual services. My Virtual Physician offers video consultations for non-emergency care to older adults and children. If you need to see a doctor, book now.
Contact us today to find out how you can book a consultation appointment.
Disclaimer: The contents of this article are for informational purposes only and do not constitute medical advice. The information, graphics, and images on this site are not intended to substitute diagnosis or treatment by a medical professional. Always seek the advice of a licensed physician for any questions you may have regarding a specific condition.
“Extreme Weather and Your Heart: What You Need to Know When It Gets Really HOT!”. secondscount.org. Accessed July 31, 2022.
“Heat Exposure and Cardiovascular Health: A Summary for Health Departments”. cdc.gov. Accessed July 31, 2022.
“Heat-related health dangers for older adults soar during the summer”. nih.gov. Accessed July 31, 2022.
"Work Clothing and Personal Protective Equipment (PPE) Elements of Your Written Program and Effective Work Practices". dir.ca.gov. Accessed July 31, 2022.
“15 Water Rich Fruits To Keep Your Hydrated in Summer | List Of Water Rich Fruits | Fruits With Highest Water Content”. seniority.in. Accessed July 31, 2022.
Sarah Falcone, BSN, RN, WCN-C, CSWD-C, is a registered nurse in Fort Worth, TX. She works with clients in home health, wound care, and telemedicine. Sarah is a passionate advocate for moving advanced levels of care to the home, where her clients can safely receive the medical treatments they need with greater satisfaction and comfort. She focuses on patient experience, outcomes, and advancing clinical models using innovative technology to serve patients better. Sarah draws from 15 years of practicing patient care and nursing leadership to share her own nursing experiences and expertise online. Connect with her on LinkedIn!
Telemedicine provides a convenient way to get the care you need without traveling to the doctor or specialist you need. Virtual care, or Telehealth, has been around for a while, but recent changes in healthcare have caused telemedicine services to surge.
In the past, telemedicine visits were used primarily as urgent care encounters. If you had symptoms of a cold, you could chat with a Tel-a-doc and maybe get antibiotics.
Today, telemedicine services have expanded. And patients can see their telemedicine doctor for gynecologic, primary, and even wound care. In this post, we will look at how telemedicine has become a solution for patients with chronic or non-healing wounds by answering these questions.
Read on to learn more about telemedicine as a wound care solution.
Telemedicine is a healthcare delivery model that involves virtual consultations between patients and physicians, using online tools such as video conferencing, virtual examination rooms, and remote medical devices.
In many situations, telemedicine is ideal for individuals with wounds.
Those injured or struggling with chronic wounds may not feel like leaving home. Or they may be physically unable to leave home without assistance.
Often their caregivers work and cannot take time from work for frequent doctor appointments. Also, depending on where an individual lives, there may not be a wound specialist in the area. If there is a local certified wound care expert, they may have limited availability.
So, wound care appointments may be difficult to get.
Telemedicine providers with specialized training and certification in wound care can save patients and their families frequent trips to their doctor or wound clinic. Telemedicine for wound care is efficient. Doctors can conduct virtual visits, see the wounds, and make treatment recommendations through video.
Telemedicine also lets patients have virtual follow-up conversations with their doctors and send images when the wounds change.
Telemedicine decreases costs by reducing the need to travel long distances to the hospital or to consult with a physician. It improves the quality of life for patients with chronic wounds while maintaining high standards of wound care.
Since the COVID-19 pandemic, federal and state programs (Medicare and Medicaid) and private insurers have expanded coverage for telemedicine services, including wound care.
That is good news for patients with wounds who need to see a specialist. In many cases, your health insurance will cover the cost of your virtual visit and wound care supplies that your provider orders.
Your insurance may cover a virtual doctor visit for treatment if you have:
You can check with your insurance company to find out what they will cover or talk with a telemedicine provider and have them verify your insurance coverage before making an appointment.
Wound care specialists provide a variety of services through telemedicine. According to the Department of Health and Human Services, Telehealth services are especially helpful for monitoring and improving ongoing health issues, like chronic wounds.
A telemedicine wound care specialist can evaluate and treat wounds virtually by:
These services help patients get the right treatment to heal the wound quickly and return to normal lives.
Telemedicine specialists also coordinate your care with your other doctors or home health.
There are many advantages of using telemedicine wound care services, including:
It’s easy to see why telemedicine wound care services are growing.
While there are numerous benefits of telemedicine for patients, primary among them is the ease of convenience and the ability to access quality care fast. Wound care services provided through telemedicine are a great example of a wound care solution that is helping many individuals get the care they need.
If you have a skin wound that needs medical attention, talk with the My Virtual Physician team to find out if their telemedicine wound care services are right for you.
Contact us now for your low-cost appointment that your insurance may cover!
Telemedicine, also known as telehealth, improves access to healthcare without being physically present at a healthcare facility. Over digital devices with an internet connection, people can speak with a doctor and get all the help they need.
Although introduced in the late 1950s, the need and use of telehealth services recently peaked during the Covid-19 pandemic. For several reasons including lockdown restrictions, fear of getting infected, and increased burden on the healthcare system, thousands of people could not leave their homes to visit a healthcare facility. While things are seemingly back to normal, telemedicine might be here to stay for good.
The question then arises, does my health insurance cover telehealth? The answer is music to the ears. Medicare covers a wide range of medical and health-related services, and that includes telehealth. In this article, we will discuss what parts of Medicare cover telehealth services.
Book Appointment Now Call For An Appointment
Medicare is made up of different parts namely:
Each of these parts covers different medical and health-related services. Telehealth is covered by Medicare parts B and C.
Medicare Part B covers outpatient services, and since telehealth visits are treated as such, it covers telehealth services. Hence, you may enjoy the services of the following health professionals:
According to the Centers for Medicare & Medicaid Services (CMS), the outpatient-related telehealth services you may enjoy include:
Additionally, the price is the same. The amount people with Medicare pay for in-person outpatient services is the same amount for telehealth services. According to the CMS, Medicare covers 80% while the personal pays 20% of the cost of standard services. Some of these healthcare services may start with an in-person visit and continue with virtual visits.
Medicare Part B can also cover emergency (ambulance) transportation and limited non-emergency rides. So, if a client with Medicare needs transportation to a healthcare facility for follow-up care, its cost may be covered. The same goes for non-emergency transportation. If a client is nonambulatory or needs monitoring in transit to another facility, the cost of transportation may be covered. Clients are to check if Medicare can cover their transportation needs.
Medicare Part C, also known as Medicare Advantage is sold by private insurance companies. In 2020, it was upgraded to provide increased access to telemedicine services from home. Generally, it has the same coverage for telehealth services as original Medicare (Part A and B) but may come with additional benefits.
Since it is provided by private insurance companies, the plans may be different. Individuals should check their specific plans with their insurance provider to know what telehealth services they are entitled to enjoy.
At My Virtual Physician, we are in-network with many insurance health plans including Medicaid, Medicare, United HealthCare, and Blue Cross.
Our team is committed to ensuring that patients get the best of health care as needed. We provide virtual care at any point in your pregnancy while you await your appointment with your local OB doctor. We are also available to help guide you through your pregnancy and answer any questions that may arise.
Book Appointment Now Call For An Appointment
Every 13 minutes, a woman dies from breast cancer. Unfortunately, many women with the disease do not show symptoms. So, regular screening for breast cancer is critical for early detection and diagnosis.
Breast Cancer screening typically occurs as a part of routine preventative care. Individuals do not have to have any signs or symptoms to have a screening performed by their doctor. Manual exams, ultrasound, thermography, and mammography are a few ways patients are screened for abnormalities. A doctor can explain screening options and when it is time to consider certain tests.
To find out how breast cancer screening aids in the diagnosis of the disease, read on.

Breast cancer can be asymptomatic. In other words, it may have no symptoms. In fact, cases may show different symptoms and examination findings. That is why screening should be individualized for each patient.
Screening means looking for or testing for something when there are no signs.
Many people think that only someone with a family history should worry. Yet, about 85% of breast cancers occur in women who do not have any family history of breast cancer. Rather, genetic mutations that occur as women age increase their risk. The most significant risk factors for breast cancer are being a woman and growing older.
Doctors are trained in the latest research and guidelines. They can tell their patients about the options. And doctors help women decide when it is a good idea to be tested.
Breast cancer is typically diagnosed in one of the following ways:
Mammography is the most common screening method used today. Other testing methods include Digital Breast Tomosynthesis (DBI) and thermography, although these are not widely used.
According to a recent article, doctors are seeing later-stage cancer cases in younger women. This is worrisome because cancers detected in younger women in their 20s and 30s are more aggressive. And they may lead to poorer outcomes.
Doctors are seeing later-stage cancer cases in younger women. This is worrisome.
Early detection is key in cancer treatment. The cost of treatment, risks of complications including death, and length of treatment go down with earlier detection.
If not caught early, cancers can grow and spread. When cancer cells move to other organs, this is called metastasis. Thus, cancer is harder to treat.
The best way to catch cancerous changes early is through regular check-ups with a doctor and routine screening tests to help detect changes early. Online doctors or virtual gynecologists can order mammograms or other imaging tests, and tailor screening plans for women who do not usually see a primary care physician.
Medical researchers continue to look for ways to help doctors with better and more accurate tests.
In 2019, the National Cancer Institute presented a new study that showed Doctors could detect breast cancer up to five years before any clinical signs appear, using a blood test for tumor-associated antigens (TAAs).
Newer research from Johns Hopkins University School of Medicine paired blood tests with other screening tests to determine whether finding and treating cancers identified by blood tests reduced mortality rates. Researchers said that “some screening may actually cause more harm than good.” And so, they used bloodwork with standard imaging procedures.
Results were promising. Researchers concluded that there is hope for a blood test that could eventually reduce deaths from cancers that typically go undetected until late stages. But “any blood test needs to complement and add to standard-of-care screening because standard-of-care screening works.”
Current recommendations encourage most women to have a mammogram beginning at age 40. Here are the most recent guidelines on screening.
My Virtual Physician can offers virtual gynecology services in many states. Women can talk with experts about individualized screening plans. Don’t worry about your risk. Talk to the doctor now.
My Virtual Physician is now accepting new patients.
Lung cancer is the second most common cancer in the United States, just behind prostate cancer in men and breast cancer in women. Lung cancer also happens to be the most lethal cancer, accounting for approximately 25% of all cancer deaths. Each year, more men die of lung cancer than from colorectal, prostate, and pancreatic cancers combined, and more women die annually of lung cancer than from breast, cervical, and uterine cancers combined.
The main risk factor for lung cancer is cigarette smoking, associated with 85% of cases. Among smokers, the risk of lung cancer increases with number of cigarettes smoked and duration of smoking history. There is good news though: the risk of lung cancer will decrease with smoking cessation and may even approach that of the nonsmoking population after 10 to 15 years of tobacco abstinence. Meanwhile, associated risks of developing lung cancer from e-cigarettes are currently under investigation.
Each year in the U.S., up to 26,0000 lung cancer deaths occur in never smokers, with an even higher proportion in some geographic areas. This brings us to environmental risk factors of lung cancer, such as exposure to radon, a chemically inert gas from uranium decay, encountered by underground miners and less commonly, residentially, through indoor exposure in the home basement. Asbestos exposure can lead to a type of lung cancer called mesothelioma and can cause other types of lung cancer when combined with smoking.
Arsenic, chromium, nickel, air pollution, and second-hand smoke represent other occupational or environmental exposures associated with lung cancer risk. Patients with treated for breast cancer, Hodgkin and non-Hodgkin lymphomas with high doses of radiation to the chest have increased risk of lung cancer, especially if they smoke cigarettes. Family history is another predictor of increased risk. Other diseases associated with increased lung cancer risk include chronic obstructive pulmonary disease and restrictive lung diseases, including fibrotic disorders like pneumoconiosis.
Finally, there have been dietary associations with lung cancer. An increased risk has been found with diets deficient in vitamins A and C, but supplementation with beta-carotene has been associated with an increased risk (in heavy smokers, the highest-risk populations, in 2 of 3 clinical trials).
On the basis of findings from the NLST trial, screening for lung cancer with low-dose computed tomography (LDCT) scan is recommended for certain patients by the U.S. Preventive Services Task Force (USPSTF). See Table 1.
Table 1. USPSTF Recommendation Summary for Lung Cancer Screening
| Population | Recommendation |
| Adults aged 50 to 80 years who have a 20 pack-year smoking history and currently smoke or have quit within the past 15 years | The USPSTF recommends annual screening for lung cancer with low-dose computed tomography (LDCT) in adults aged 50 to 80 years who have a 20 pack-year smoking history and currently smoke or have quit within the past 15 years. Screening should be discontinued once a person has not smoked for 15 years or develops a health problem that substantially limits life expectancy or the ability or willingness to have curative lung surgery. |
Adults aged 50 to 80 years have a 20 pack-year smoking history and currently smoke or have quit within the past 15 years should screen for lung cancer with LDCT every year. A pack-year is a way of calculating how much a person has smoked in their lifetime. One pack-year is the equivalent of smoking an average of 20 cigarettes (1 pack) per day for a year. These recommendations are available at www.uspreventiveservicestaskforce.org.
If you would like to learn more and connect with a board-certified physician, click to book now on My Virtual Physician. My Virtual Physician offers comprehensive medical services where you can discuss the best screening plan for you with a virtual doctor.
References
https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening
Siegel RL, Miller KD, Jemal A: Cancer statistics, 2019. CA Cancer J Clin 69: 7-34, 2019. PMID: 30620402.
Jemal A, Thun MJ, Ries LA, et al: Annual Report to the Nation on the Status of Cancer, 1975-2005, featuring trends in lung cancer, tobacco use, and tobacco control. J Natl Cancer Inst 100:1672-1694, 2008. PMID: 19033571.
Omenn GS, Goodman GE, Thornquist MD, et al: Effects of a combination of beta carotene and vitamin A on lung cancer and cardiovascular disease. N Engl J Med 334:1150-1155, 1996. PMID: 8602180.
Menkes MS, Comstock GW, Vuilleumier JP, et al: Serum beta-carotene, vitamins A and E, selenium, and the risk of lung cancer. N Engl J Med 315: 1250-1254, 1986. PMID: 3773937.
Alpha-Tocopherol, Beta Carotene Cancer Prevention Study Group: The effect of vitamin E and beta carotene on the incidence of lung cancer and other cancers in male smokers. N Engl J Med 330:1029-1035, 1994. PMID: 8127329

More than 100 million Americans are living with abnormal blood sugar. Is it possible that you could be one of them? A simple A1c screening blood test shows when levels are too high. Elevated blood sugar means higher risk for diabetes.
A glycated hemoglobin, or hemoglobin A1C, test (HbA1c) is one screening test that checks blood sugar levels. Results show how much sugar is in the bloodstream over time. Testing is accurate since values are not affected by acute illness or stress. A1c screening is recommended for certain populations, including overweight adults and those with other risk factors.
Those thinking about blood sugar testing or wondering about risk factors should talk to their doctor. Here are some common questions about diabetic screening and A1c testing.
The A1c test can detect diabetes because it measures how much sugar, called glucose, is found in red blood cells. The red blood cells give a “glycemic history” of the past 120 days.
Everyone has sugar in their blood. But diabetics have higher levels. Blood sugar that is too high leads to cell and tissue damage.
When someone is diagnosed with diabetes, their doctor will also use the A1c test to monitor how the disease is being controlled.
A1c readings are measured in percentage. Here is what A1c results mean.
Higher blood sugar levels cause greater A1c values, and they equal greater risk for diabetes.
Early detection is key in diabetes because early treatment can prevent serious complications. When a problem with blood sugar is found, doctors and patients can take steps to prevent permanent damage to the heart, kidneys, eyes, nerves, blood vessels, and other vital organs.
Here are the current recommendations for A1c screening.
The CDC suggests A1c screening to know a baseline for:
They further recommend that any woman who has ever had gestational diabetes should have an A1c check every three years even if results are normal.
The USPTF also says that adults over age 45 should be checked for diabetes using the A1c test. Furthermore, it recommends repeat testing every three years.
The ADA also recommends the A1c test, or other diabetic screening, for all adults at age 45 and over. Additionally, it advises overweight individuals with one or more risk factors to be screened, regardless of age. If results are normal, repeat screening is recommended every three years or less.
How to Get an A1C Test
If you meet some of these guidelines, you might be wondering how you can get a screening test.
A primary care doctor or other licensed provider can order this common blood test. Results take as little as a few business days.
Those who do not have a doctor to order the test, can still get this valuable screening. An online doctor or virtual physician can help. Telemedicine providers work with laboratory partners to treat patients without unnecessary trips to an office.
An online physician sends referrals and lab orders just like a brick-and-mortar doctors office. After going to a lab for blood work, virtual doctors offices schedule follow up video visits to go over the results, answer questions, and discuss treatment plans.
If you would like to talk with one of our board-certified physicians, book and appointment today. My Virtual Physician offers health screening, lab tests, and counseling to meet all of your healthcare needs.
If you have suggestions for other topics you want to read about, let us know! Don’t forget to follow us on social media.
In the United States, colorectal cancer (CRC) is the third leading cause of cancer, after breast and lung cancer.
CRC almost always develops from precancerous polyps (abnormal growths in the colon or rectum). Screening tests can find precancerous polyps so they can be removed before they turn into cancer. Screening tests can also find CRC early, when treatment works best.
A screening test is used to look for a disease when a person has no symptoms. (When symptoms are present, diagnostic tests are used to find out the cause.)
Regular screening begins at age 45. The U.S. Preventative Services Task Force (USPSF) recommends adults age 45 to 75 be screened. For adults age 76 to 85, the Task Force recommends asking their doctor for screening recommendations.
Talk to a virtual doctor today!
Several screening tests can be used to find polyps and/or CRC (see Table 1 below). There is no single “best test” for any person. Each test has advantages and disadvantages. Talk to a virtual doctor about which test may be best for you and how often to be tested. Testing modality depends on personal preference, individual medical conditions, the likelihood of testing, and the resources available for testing and follow-up.
Table 1. Screening Tests for CRC
| Test Name | Description | Testing Frequency |
| Stool TestsGuaiac-based fecal occult blood test (FOBT) | Uses the chemical guaiac to detect blood in stool. Test provided by health care provider. At home, use a stick or brush to obtain a small amount of stool. Return the test kit to doctor or lab, where stool samples checked for presence of blood. | Once a year. |
| Fecal immunochemical test (FIT) | Uses antibodies to detect blood in stool. | Once a year. |
| FIT-DNA test (or stool DNA test) | Combines the FIT test with a test that detects altered DNA in the stool. This test requires an entire bowel movement be collected and sent to a lab, where it is checked for cancer cells. | Once every 3 years. |
| Flexible Sigmoidoscopy | During this test, the doctor inserts a short, thin, flexible, lighted tube into the rectum through the sigmoid colon (lower 1/3 of colon). The doctor checks for polyps or cancer there. | Every 5 years, or every 10 years with a FIT every year. |
| Colonoscopy | Similar test to flexible sigmoidoscopy, except the doctor uses a longer, thin, flexible, lighted tube to check for abnormalities inside the rectum and entire colon. During the procedure, the doctor can find and remove most polyps and some cancers. Colonoscopy is also used as a follow-up test if anything unusual is found during one of the other screening tests. | Every 10 years (for people who do not have an increased risk of colon cancer). |
| CT Colonoscopy (Virtual Colonoscopy) | Computed tomography (CT) colonography, also called virtual colonoscopy, uses X-rays and computers to produce images of the entire colon. These are displayed on a computer screen for the doctor to analyze. | Every 5 years. |
The screening testing frequencies above are general guidelines and may be different for you if you have certain risk factors for CRC, such as a family history of CRC or detection of high-risk lesion. Testing is generally more frequent for patients who are high risk. Your doctor will help you decide the optimal screening interval.
Connect with Our Online Doctors
If you would like to connect with a board-certified physician, book an appointment with a virtual doctor today. My Virtual Physician offers comprehensive medical services where you can discuss the best screening plan for you
Sexually transmitted diseases (STDs), also called sexually transmitted infections (STIs), are very common, with around 25 million new diagnoses made yearly in the United States. Young people, ages 15-24 years of age, appear to be the most prevalent group to acquire and spread STDs, accounting for about half of newly diagnosed cases in 2018 per the Centers for Disease Control (CDC). Notably, 1 in 5 people in the United Stated have had an STD.
Oral, vaginal and anal sexual encounters are the methods of transmission and these infections vary greatly in their symptoms, severity, curability and prognosis. Treatment has improved over the years and some lifelong conditions now do not preclude a good quality of life. However, some of these diseases can be quite quiet in terms of initial symptoms, and screening tests, or tests to check if a disease is present even when symptoms are not, are a critical way to help reduce transmission and consequences of these infections.
Bacterial Vaginosis, not categorized itself as a sexually transmitted disease, is a condition named for alterations in the normal balance of bacteria in the vagina, which can lead to an increased risk for susceptibility to STDs, as well as preterm labor. A fishy odor may be noted after vaginal intercourse, and pain, itching and burning in this area or during urination, as well as thin, grey-white vaginal discharge, are among associated complaints. Although many cases of bacterial vaginosis clear on their own, antibiotic treatment may be needed at times. Currently, there is no recommendation for routine screening for BV.
Two of the most predominant, but easily treatable STDs, include chlamydia and gonorrhea. Both can spread through oral, vaginal or anal sex. Though either condition may be asymptomatic, some suspicious findings include abnormal vaginal or penile discharge, burning while urinating and pain or swelling of the testicles. Chlamydia and gonorrhea can also reoccur if infectious sex continues, despite prior treatment. Also, having these infections increases a woman’s risk to develop pelvic inflammatory disease (PID), which is damage to the internal reproductive organs, making future fertility a challenge. If infected during pregnancy, risk for miscarriage, preterm labor, low birth weight or an infection in the fluid surrounding the fetus, called chorioamnionitis, increases. Newborns of untreated mothers may also suffer postnatal complications such as eye infections and pneumonia. Pregnant women < 25 years of age, or older pregnant women at increased risk of exposure to gonorrhea or chlamydia, are typically screened at their first prenatal visit. Similarly, it is recommended to screen all sexually active women < 25 years of age, yearly, for gonorrhea and chlamydia, and older women who have multiple sexual partners. All sexually active gay or bisexual men, should also be screened at least yearly, but more often depending on frequency of new sexual encounters/multiple partners. Testing for these diseases can be as simple as a urine sample ordered by a virtual physician, however it is prudent to discuss symptoms and history to determine the best course of screening.
According to the CDC, every 1 out of 6 people in the United States has herpes simplex virus (HSV) infection, oftentimes without knowing it. HSV can be divided into HSV 1, more commonly known as oral herpes, and HSV 2, known as genital herpes. Although designated as such, either can occur orally or genitally. Many people are infected with HSV 1 in their childhood, through non sexual mediated contact with infected saliva. Oral herpes results in cold sores or fever blisters, around the lip and mouth area. Genital herpes, likewise, can demonstrate sores throughout the genital region of infected individuals. Lack of active sores however does not negate infectious activity and the disease can still spread through unprotected oral, vaginal and anal routes. There is no curative treatment for HSV and the virus can go into a dormant phase where no symptoms occur for years, though patients are at risk for recurrent outbreaks, where an antiviral medication may be prescribed. Devastating effects can occur if left untreated during pregnancy, including life-threatening infection to the newborn. If there is history of infection or active infection at the time of labor, a Cesarean section may be indicated. The United States Preventive Services Task Force does not recommend routine screening for HSV in asymptomatic sexually active adolescents or adults, including pregnant women.
Syphilis is a bacterial infection spread through sexual contact, and is divided into distinct phases, first beginning as painless mouth/oral, genital or anal sore(s) several days to several months after initial exposure. This sore or sores will resolve after a few weeks, even without medication. Then a body rash develops, sometimes with swollen lymph nodes, general fatigue and a fever, later. There can be a long period of “latency”, or no symptoms, followed by the last stage classified by neurological, ocular and cardiac symptoms. This is a curable condition, but can cause life-long consequences if untreated, including dementia and blindness, and can lead to death. Screening is indicated for sexually active individuals on a yearly basis, but more often such as every 3-6 months for high risk features, such as multiple partners. This can be performed through a blood test, which may be ordered through a virtual physician’s visit.
Although there are other methods of transmission, typically hepatitis B may be acquired through the sexually transmitted routes mentioned above. Hepatitis C is less commonly sexually transmitted, but spreads through exposure of infected blood, such as in activities like sharing needles in illicit IV drug abuse. Both conditions, though incited by different viruses, have the same impact on the liver and symptoms can overlap, with fever, fatigue, yellowing of the eyes and skin, abdominal pain and changes in urine color. With the exception of individuals living in extremely low prevalence areas, it is recommended that hepatitis C screening be given to a person at least once after the age of 18 years. Additionally, although hepatitis B is a vaccine preventable illness, the USPSTF recommends screening by blood test, those individuals at high risk such as those who inject drugs or share needles, men who have sex with men and immunocompromised patients, such as those with HIV, as well as those living in areas with a 2% or higher prevalence of the hepatitis B surface antigen, regardless of vaccination status. This is especially important given that hepatitis B is a chronic illness that will need lifelong treatment and both viruses present a higher susceptibility to liver cancer.
HIV, or human immunodeficiency virus, eventually progresses to acquired immunodeficiency syndrome (AIDS). Fortunately, through screening and early detection, appropriate prophylactic and supportive agents can be provided to help maintain CD4 counts and stable immune status in order to prevent, or at least slow, this advancement. It is generally recommended that adolescents beginning at 13 years, through adulthood, into the 60s, be screened via blood test, at least once as part of routine health maintenance. For those in higher risk categories, such as individuals with multiple sexual partners, men who have sex with men and those who share needles, screening may be advised yearly or with more frequent intervals depending on individual circumstances. Once again, this is a blood test that may be ordered through a virtual doctor visit.
While prevention of any illness is optimal through regular visits with a physician, screening tests have proven to be useful in early detection of otherwise asymptomatic diseases, allowing for quicker treatment. In particular, sexually transmitted diseases are relatively easy to screen for through blood or urine samples. If you have questions or concerns regarding your need to be screened for these conditions, it is quite simple to schedule a virtual visit with one of our physicians at My Virtual Physician, and we can help determine which testing is right for you. In addition, depending on the results, oftentimes follow up guidance or medication can also be provided! Schedule a visit today!
Half of adults over the age of 50 are at risk for broken bones. Maintaining healthy bones is important for a long healthy life.
Osteoporosis (OP) is a condition of weakened bones. Thin bones are at risk for fractures. OP screening can be an important part of staying healthy. Early disease detection and treatment may prevent complications later. Broken bones are painful and costly. Luckily, screening tests like the Dual-Energy Xray Absorptiometry (DEXA) scan alert doctors of problems early.
DEXA scans or other OP screening tests are advised for some at-risk groups. To find out if you should be concerned about bone testing today, read on.

OP is more common in adults than you may believe. One health department called it a major public health threat.
OP screening may prevent:
People with OP may not know anything is wrong until they suffer an injury. With advanced bone disease, normal activities can cause bones to break. Studies have shown that many patients do not get the right treatment for low bone density (LBD) despite the great prevalence, complications, and costs of fractures related to bone disease.
Therefore screening tests for bone loss are important to your health. Doctors or specialists can diagnose problems with weak bones before they become serious.
OP affects one-in-three women above 50 years old. It is also a serious condition for men.
It is best to talk to a doctor about when to get a screening test. They can explain the test and treatment options. Physicians will also answer questions about what to expect.
Currently, we have a few recommendations for OP screening.
The NOF advises a DEXA scan of the hip and spine for:
Also, they also encourage testing in those with:
The ISCD has similar guidelines. They recommend DEXA scan of the hip and spine for the same groups above, but also in:
AACE recommends a DEXA scan for
The AACE says that the lumbar spine and proximal femur are the best sites for testing.
The USPSTF recommends screening for OP in women 65 years or older. Also in younger women with certain risk factors. At this time the USPSTF does not have a recommendation for men.
ACOG currently urges screening for women 65 or older and those under age 65 with risk factors for fracture. They also say physicians should screen patients using the FRAX tool to define their risk of a major fracture.
The FRAX® tool evaluates fracture risk in patients. Based on the score, a 9.3% or higher risk should be referred for a DEXA scan.
The DEXA scan is a quick and reliable test for measuring bone mineral density (BMD). It aids in the diagnosis of OP.
The scan usually takes around 15 minutes. And it doesn't hurt. First, the patient lies down on an open table.
Next, a scanner passes over the body. It sends two X-ray beams. And the machine tells how the rays pass through the bones. This shows how thick or thin they are. The results give the doctor a good idea of how healthy the bones are.
Like other medical tests, a DEXA scan is ordered by a healthcare professional. Typically, doctors or specialists can write a prescription or send a referral. Virtual doctors and online physicians can also arrange this test for their patients.
OP screening may be a part of your yearly check-up. Or it can be used to check on certain risk factors.
Thanks to telemedicine, it is now fairly easy to get this important test. An online doctor can tell you about OP screening and answer your questions. Online appointments are convent. Patients meet doctors from wherever they are, on a mobile device or smartphone.
My Virtual Physician offers screening consultations at little or no out-of-pocket cost. They can order blood tests, imaging or scans, X-rays, and more. And in some cases, same-day appointments are available.
Many screening tests are covered by health insurance or medical benefits. Check with your insurance to see if any out-of-pocket payment is required. Medicare pays for bone density testing every two years for adults over 65 with some risk factors.
My Virtual Physician offers full preventive care services for men and women. To talk with one of the top physicians, click to book an appointment now. The MVP caring experts help patients with screening plans that are tailored to their healthcare needs.
If you have ideas for other topics you want to read about, let us know! Don’t forget to follow us on social media.
Sources:
Breast cancer is now the most common cancer in the world. In fact, 12% of all new cancer cases in 2021 will be breast cancer. As a result, chances are you know someone who has faced this terrible disease. And it is likely you have wondered about breast cancer screening.
Currently, there are several recommendations about breast cancer screening. There are benefits to screening and early detection, but there are also potential problems. Your doctor should help you decide which tests you need based on your history and risk. For high-risk men and women with a family history of cancer, BRCA genetic testing is invaluable.
Breast cancer screening is a great way to take charge of your health. Here's what you need to know about breast cancer screening.

According to the National Cancer Institute, screening means looking for the disease before there are any signs. Hence, the best time to get checked is before you have symptoms.
Screening is looking for abnormalities. It may find cancer at an early stage. Because of advanced detection, doctors can more easily treat the disease. Patients also have better odds at survival. Each type of cancer has unique guidelines for screening.
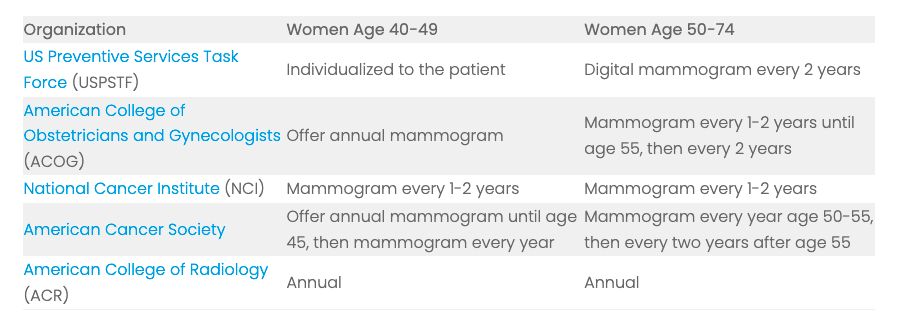
Overall, current guidelines and recommendations say that most women should have a mammogram to detect tissue changes beginning at age 40.
Men are also affected by breast cancer. However, most guidelines do not include them in the recommendations. A doctor can give male patients personalized guidelines for screening.
Here are the most current routine recommendations for women starting at age 40.
| Organization | Women Age 40-49 | Women Age 50-74 |
| US Preventive Services Task Force (USPSTF) | Individualized to the patient | Digital mammogram every 2 years |
| American College of Obstetricians and Gynecologists (ACOG) | Offer annual mammogram | Mammogram every 1-2 years until age 55, then every 2 years |
| National Cancer Institute (NCI) | Mammogram every 1-2 years | Mammogram every 1-2 years |
| American Cancer Society | Offer annual mammogram until age 45, then mammogram every year | Mammogram every year age 50-55, then every two years after age 55 |
| American College of Radiology (ACR) | Annual | Annual |
Some men and women worry about breast cancer because they have a family history of cancer.
Women with a personal or family history of some cancers could have changes in their genes. These mutations are known as BReast CAncer gene 1 (BRCA1) or BReast CAncer gene 2 (BRCA2) changes. They may mean a higher cancer risk.
High-risk patients should see a doctor or specialist. They will need a risk assessment, genetic counseling, and in some cases, lab testing. Mutations in the BRCA1/2 genes may lead to:
Genetic testing for BRCA1/2 requires a special blood test that your doctor can order. The doctor can explain the details. They can also answer questions you might have.
According to the National Cancer Institute, many women with ovarian and breast cancers are not receiving these genetic tests, even though they have become inexpensive and easily accessible.
Now with telemedicine, it is easier than ever to get this valuable testing done. An online provider such as a virtual gynecologist or virtual physician can tell you if you need it and when or how to get it.
My Virtual Physician offers consultations about this important BRCA gene testing. For little or no out-of-pocket cost, they can arrange for you to have your blood drawn. They make it easy. They work with many local LabCorp or Quest outpatient testing centers who can provide this service for you.
Like much in healthcare, tests may not be “one risk fits all.” That is why you should talk to your doctor about what is best for you. He or she will consider factors such as lifestyle, family history, and other health concerns. Then they can help you decide what to do.
Your doctor can recommend one of these methods below. If you do not have a doctor, a virtual doctor online can be a great place to start.
The most common test for breast cancer is called mammography. It is ordered by a doctor. Mammograms look for early changes in the tissue that could be dangerous.
A mammogram is a special type of X-ray that shows the breast tissue. Sometimes, doctors can see lumps on the images that they cannot feel.
Women who have a high risk of cancer or have dense breast tissue may require magnetic resonance imaging.
The MRI test is more sensitive and can detect finer irregularities. MRI images also give a clearer picture of the breast tissue. Unfortunately, this screening method is much more expensive and therefore is not used for routine exams.
Breast cancer testing is an active area in clinical research. Other methods include:
Physicians can explain the options to patients. And they can help them make informed choices about each type of screening.
Doctors can help guide a patient to the best choice. Physicians also tell their patients about risks that they need to consider.
Your doctor should tell you when to get screened for breast cancer. Talking to a board-certified physician about the right time for you to have a cancer screening may prevent problems.
Specialists caution patients that there are risks involved with all medical tests, including cancer screening. Some of them include:
This is why you should talk to your doctor when you are thinking about breast cancer screening.
My Virtual Physician offers a full line of virtual physician services. To talk with one of our board-certified physicians, click to book now. Our caring experts can talk with you about a screening plan that is best for you.
If you have suggestions for other topics you want to read about, let us know! Don’t forget to follow us on social media.
Sources:
Breast Cancer Overtakes Lung As Most Common Cancer - WHO. Reuters. Feb 2, 2021. https://www.reuters.com/article/health-cancer-int/breast-cancer-overtakes-lung-as-most-common-cancer-who-idUSKBN2A219B
Cancer Screening Overview (PDQ®)–Patient Version. National Institute of Health. National Cancer Institute. Aug 19, 2020. https://www.cancer.gov/about-cancer/screening/patient-screening-overview-pdq
Breast Cancer Screening. U.S. Preventative Task Force. Jan 11, 2016.https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/breast-cancer-screening
Breast Cancer Risk Assessment and Screening in Average-Risk Women. American College of Obstetricians and Gynecologists. Practice Bulletin. Number 179. July 2017. https://www.acog.org/clinical/clinical-guidance/practice-bulletin/articles/2017/07/breast-cancer-risk-assessment-and-screening-in-average-risk-women
American Cancer Society Guidelines for the Early Detection of Cancer: Breast Cancer. American Cancer Society. Jul 30, 2020. https://www.cancer.org/healthy/find-cancer-early/american-cancer-society-guidelines-for-the-early-detection-of-cancer.html
New ACR and SBI Breast Cancer Screening Guidelines. American College of Radiology. Apr 4, 2018. https://www.acr.org/Media-Center/ACR-News-Releases/2018/New-ACR-and-SBI-Breast-Cancer-Screening-Guidelines-Call-for-Significant-Changes-to-Screening-Process
BRCA Overview. Basser Center for BRCA, Penn Medicine. Accessed Jul 24, 2021. https://www.basser.org/brca
Chen, S., Parmigiani, G. (2007). Meta-Analysis of BRCA1 and BRCA2 Penetrance. Journal of Clinical Oncology, 25(11), 1329-1333. https://doi.org/10.1200/JCO.2006.09.1066
Fewer Women with Ovarian, Breast Cancer Undergo Genetic Testing than Expected. National Cancer Institute. Apr 9, 2019. https://www.cancer.gov/news-events/cancer-currents-blog/2019/ovarian-breast-cancer-testing-inherited-genetic-mutations
BRCA1 and BRCA2 Testing. BreastCancer.org. Sep 21, 2020.https://www.breastcancer.org/symptoms/diagnosis/brca
Pediconi, F., & Galati, F. (2020). Breast cancer screening programs: does one risk fit all?. Quantitative imaging in medicine and surgery, 10(4), 886–890. https://doi.org/10.21037/qims.2020.03.14

There really are few things worse than feeling gastrointestinal distress. Nausea,
vomiting and diarrhea can easily stop the most active and symptom-refractory
person cold in their tracks. While there are numerous possible reasons behind
these unpleasant feelings, we will take a look two different etiologies that
frequently get confused: viral gastroenteritis (stomach virus) and food poisoning. Let's check out
the differences.
Viral gastroenteritis (VGE), commonly dubbed the "stomach flu", is named aptly,
as it is caused by a viral infection. Typical symptoms can include fever, vomiting,
diarrhea and abdominal cramps, and they occur about 1-2 days post-exposure to
the responsible virus.
Rotavirus and norovirus are two of the most common viral bugs that cause VGE,
and both are highly contagious. In fact, prior to the development of the rotavirus
vaccine for children, rotavirus was the leading cause of gastroenteritis in children
globally, infecting nearly all young children before their fifth birthday. Because of
their smaller size and weight, significant diarrheal losses can greatly increase risk
for death by dehydration in children, which prompted initiation of the rotavirus
vaccine. Norovirus is flagged as the offending virus in about half of all VGE
cases and is also the culprit of about 90% of diarrheal epidemics around the
world.
These viruses transmit through fecal-oral fashion, or more simply, a person
becomes sick after swallowing infected stool. If trace amounts of fecal matter
remain on a person's hands, on commonly touched objects or even on food,
there is risk for spreading infection. As could be expected, hand washing is most
critical in prevention. Also, staying away from others during the peak of your
symptoms is important, but also take note that you can pass the virus on through
stool shedding that may last up to 14 days after symptoms have resolved. And it
is recommended to vaccinate young infants with the rotavirus vaccine series,
shown to have approximately 90% efficacy in prevention of severe rotavirus
infection.
Speak to a Virtual Doctor Today!
Due to similar symptoms, food poisoning often gets lumped in with the “stomach
bug”. Interestingly, food poisoning may also be caused by a virus, but is more
frequently the result of bacterial toxins or parasites. You’ve probably heard of the
advice, don’t eat raw cookie dough, because of the uncooked eggs. Other
sources for these bugs include raw or undercooked meat products,
unpasteurized dairy as well as seafood, unwashed produce and surprisingly,
flour. So essentially, these pathogens cross over different dietary staples, and
can cause similar feelings of gastrointestinal upset, body aches and fatigue, with
or without fever.
Sometimes, certain bacterial strains, such as Shiga toxin-producing E. coli
(STEC), can cause damage to blood vessels and lead to kidney injury and
failure. The diarrhea that accompanies food poisoning typically presents after a
few hours from the time of exposure and can often be bloody as compared to a
simple viral gastrointestinal illness.
Most cases of food poisoning resolve fairly quickly, within a day or two, as the
offending bug works its way out of the system. Properly storing, washing,
handling and cooking food products are the best means of prevention.
As noted above, one of the biggest concerns with VGE and food poisoning is the
risk for dehydration. Replacing fluid loss is important, focusing on water and
electrolyte replenishment. Water is usually best, however low sugar sports drinks
and pedialyte are also good options. While vomiting is still an active symptom,
taking small sips of fluids more frequently is most helpful to keep hydration in
balance. Alternatively, for those who can’t tolerate sips well, low sugar popsicles
or ice chips can work. Once symptoms have started to subside, increasing food
intake should be done slowly and intentionally. Going to your favorite fast food
drive through the day after GI symptoms is probably not in your stomach’s best
interest, as recovery is still underway, and greasy, processed food may counter
that process. Most physicians have navigated away from a traditional bland diet,
such as the often-referred to BRAT (bananas, rice, applesauce, toast) diet that
many pediatricians once advised, due to the lack of nutrition. Concentrate on
food choices that include healthy fats and plenty of protein and fiber, which can
be found in fruits and vegetables as well as whole grains.
Both viral gastroenteritis and food poisoning are often mild and self-limiting
illnesses (meaning they do not require medical intervention to resolve).
However, symptoms that should prompt a doctor’s attention would include
changes in stool color including blood in the stool, changes in breathing patterns
or difficulty breathing, pink or red urine, severe pain, worsening fatigue or
irritability in young children, or lingering symptoms such a fever, vomiting or
diarrhea that don’t abate within a few days.
As always, if you have any concerns, the online physicians at My Virtual
Physician, make it quick and convenient to help you! An online visit is easy to
arrange and we can help with guidance as well as testing, if necessary.
Schedule a visit today!