In today's fast-paced world, the importance of accessible and high-quality health care cannot be overstated. At My Virtual Physician, we are committed to revolutionizing the way patients receive medical care, making it more convenient, efficient, and effective. As we continue to grow and innovate, we are excited to announce our RegCF (Regulation Crowdfunding) campaign and we would love for you to be a part of this unique transformative journey.
Dr. David Howard, the visionary, founder, and sole stakeholder, has remarkably bootstrapped My Virtual Physician while balancing demanding hours in a hospital's labor and delivery department. Over the past four years, Dr. Howard's dedication and strategic growth efforts have propelled the company to achieve sustainable and substantial success.
Dr. David Howard was born in Jamaica and immigrated to the U.S. at eighteen years old. Dr. Howard received his Bachelor of Arts in Psychology from the Johns Hopkins University and then pursued his Md and Ph.D. in Epidemiology through the Medical Scientist Training Program at the Johns Hopkins School of Medicine.
My Virtual Physician is a national, multi-specialty telehealth company that connects patients with board-certified and licensed physicians through its secure, user-friendly virtual platforms. Our services span various specialties, including primary care, pediatrics, women's health (Gynecology), and more, ensuring comprehensive healthcare solutions for individuals and families across the US.
The healthcare landscape is rapidly evolving, and the demand for telehealth services has never been greater. By launching a RegCF campaign, we aim to:
1. Expand Our Reach: With your support, we can extend our services to underserved communities, providing vital healthcare access to those who need it most.
2. Enhance Technology: Investing in cutting-edge technology will enable us to offer even more innovative solutions and improve patient experiences and outcomes.
3. Grow Our Team: By attracting top talent in the medical and technological fields, we can continue to deliver exceptional care and drive forward our mission of making healthcare more accessible.
Participating in our RegCF campaign means contributing to a future where quality healthcare is
within everyone's reach.
This year our goals are to:
1. Develop New Services: Expand our national reach by adding even more specialty services to offer our patients.
2. Improve Patient Experience: Enhancing our virtual platform and website to ensure seamless and efficient consultations.
3. Foster Community Health: Create initiatives and partnerships that promote health and well-being in underserved communities.
Getting involved in our RegCF campaign is straightforward and accessible. By visiting our campaign page https://netcapital.com/companies/myvirtualphysician, you can learn more about our mission, vision, and growth plan. Your support, whether large or small, will make a significant difference in helping us achieve our goals.
Join Us in Shaping the Future of Healthcare
Thank you In Advance For Your Support,
David L. Howard, M.D., PH.D, CEO, OBGYN
Our previous post covered a brief introduction into what GLP-1 receptor agonist medications are. In this post we will expand a little further on the three main injectable GLP-1 medications on the market: liraglutide, semaglutide, and tirzepatide.
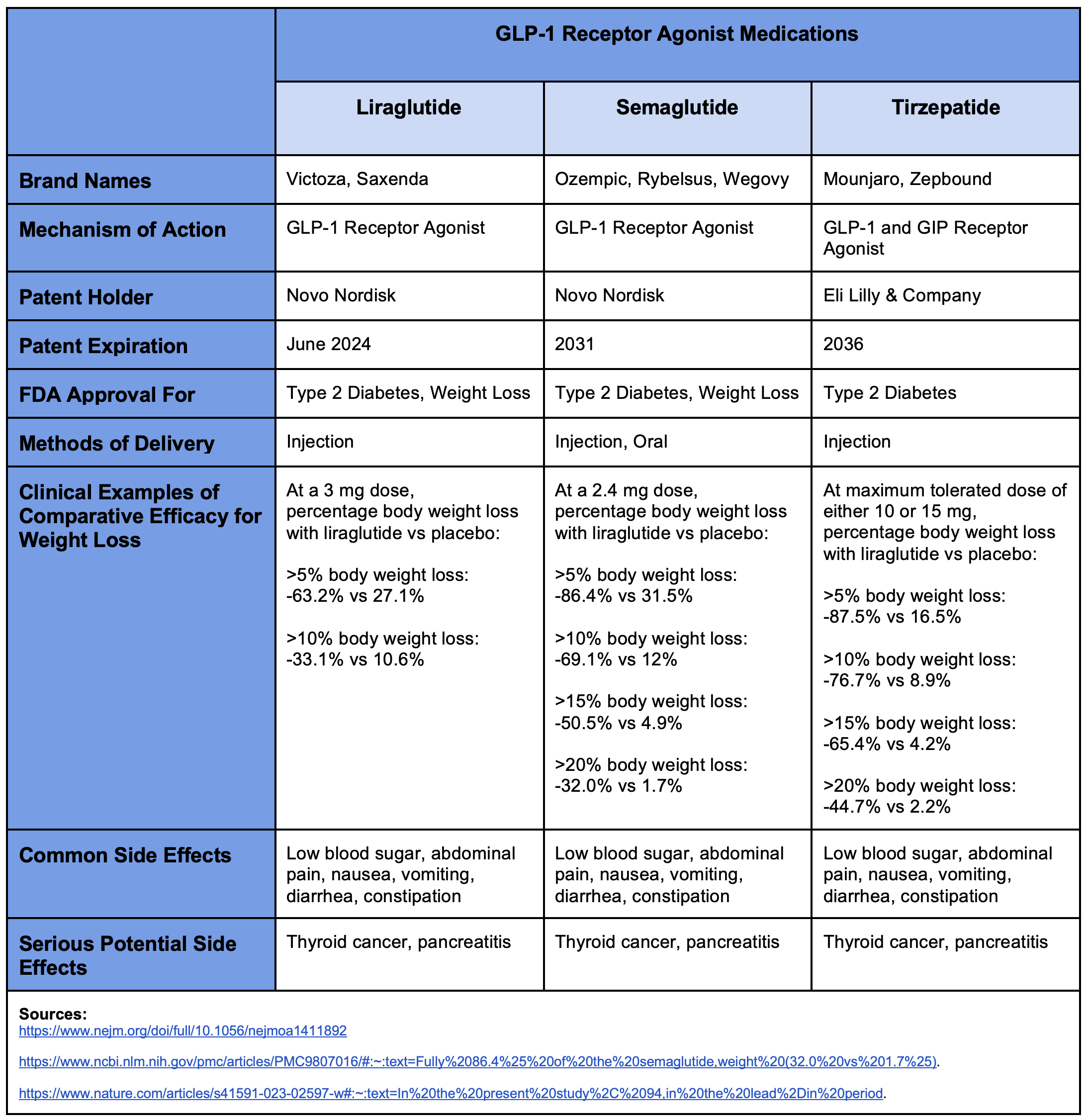
With regards to weight loss (as can be seen in the table), tirzepatide appears to perform the best of the three and liraglutide appears to be the least effective. For example, if we look at patients who successfully lost at least 10% of their body weight, we see that 76.7% of those on tirzepatide achieved this goal, 69.1% of those on semaglutide achieved it, and only 33.1% of those on liraglutide achieved it. The results for those in the placebo groups were all roughly comparable across all three drugs, thus suggesting that this is a roughly fair comparison. As one might expect, they all have fairly similar side effect profiles. And importantly of note, they all carry a potential risk of causing or exacerbating thyroid tumors. Consequently, patients with a personal or family history of thyroid cancer should make sure to discuss this with their physician before taking any of these medications.
In order to accurately consider the true cost-benefit ratio of medication you need to know the actual cost. Pricing for prescription medications is notoriously and deliberately obscure. The actual prices paid can vary enormously from state to state, from pharmacy to pharmacy, with different insurance companies, and even if you self-pay out of pocket. It can be surprisingly difficult to get a straightforward “universal price” for a prescription medication. The current “list prices” (like an MSRP) for liraglutide, semaglutide and tirzepatide are all roughly around $1,000 to $1,300 per month. And, as mentioned previously, there is not currently a generic version of any of the three GLP-1 receptor agonists we have been discussing. Consequently, while it is difficult to state the exact price at any given time, there currently is not a strong cost benefit to any of them versus the others.
However, as noted previously, liraglutide’s patent is set to expire in June of this year (2024). That means that we can reasonably expect a generic version to hit the market shortly thereafter. So, to answer the title question of whether or not there is a generic version of Ozempic, the answer is: “No, not quite yet in February 2024. But also yes, one of its major competitors should have a generic option later in 2024.” Once a generic option of liraglutide is on the market, its price will likely drop dramatically in short order. And as more generic manufacturers start producing liraglutide, the faster the price will decrease.
While it is regrettable that liraglutide seems to be the least effective of the GLP-1 medications for weight loss, it will also soon be the least expensive of them BY FAR -- and for the foreseeable future until semaglutide’s patent expires in 2031! Nevertheless, liraglutide is still undeniably an effective medication for weight loss and already has an FDA approval to be used as such. Furthermore, it is likely to cost a fraction of its competitors in late 2024. Consequently, it is highly probable that liraglutide will soon become the most cost effective medication for treating obesity within the not too distant future.
Lengthy hospital stays are often infamously derided for their seemingly exorbitant price tags, unsavory-yet-overpriced food, and general patient dissatisfaction with their perceived level of quality of care. In all honesty, these sentiments --while potentially valid-- are also often somewhat unfair, and worsened by a lack of transparency and understanding of the basic economics that go into maintaining a viable hospital system operational, particularly within our current medico-legal environment. All that notwithstanding, there are very legitimate reasons for someone to search for alternative solutions to long-term care that are better suited to both the patient and their family’s lives. One of these potential alternatives is “hospitalization” at home.
Many hospitals and emergency departments (EDs) across the country are facing serious shortages of available hospital beds for inpatient care. As a result, many ED’s are stuck “boarding” patients in hallways for days or even weeks while they await a hospital bed to open up. Obviously, this is less than ideal for myriad reasons: it is uncomfortable and unpleasant for the patient; it increases potential exposure to pathogens and the development of new hospital-acquired infections; it increases wait times in EDs; and so forth.

Fortunately, the Centers for Medicare and Medicaid Services (CMS) actually have expanded their Hospitals Without Walls initiative by creating the Acute Hospital Care at Home (AHCAH) program, which financially covers “hospitalization” at home. This program allows patients to remain in their homes with daily follow-up by healthcare providers, as the situation warrants. This daily follow-up can range from in-person nurse or physician visits (to administer medications, maintain intravenous (IV) lines, perform examinations, etc,), all the way to even virtual check-ins by a clinician to make sure everything is going well.
As one would assume, there are limitations to this program. The patient must be sufficiently ill to have otherwise warranted normal hospitalization. However, their condition must also be sufficiently low in severity and stable that they do not require immediate access to the lifesaving resources found in a physical hospital. The patient must be able to perform the basic activities of daily living, or at least have reasonable assistance available for certain limitations. Furthermore, admittance to the program requires an in-person evaluation from a physician. This can be performed in an ED or community clinic, where the physician determines the individual warrants hospitalization, but is safe to be admitted to the home hospitalization program. Alternatively, if the patient is already admitted to the hospital, their hospital physician may determine that they are stable enough to continue their “hospitalization” at home. The home must also be assessed to ensure it is a safe environment and meets basic criteria such as running water, indoor plumbing, heating and/or air conditioning, etc. A member of the clinical team must also meet with the patient at their home to go over the entire treatment plan and assess what additional steps might need to be taken (such as providing meals, for example).
Ideally, this program should offer greater convenience and comfort to suitable patients, while also reducing the inpatient costs and overcrowding burdens on the healthcare system. There are currently 53 health systems with 116 hospitals located across 29 states that have been approved for this program. To see if a hospital near you is participating in the program, you can check the following list published by CMS.
Theoretically, home hospitalization programs could help alleviate hospital crowding and extended ED “boarding” stays, in addition to possible savings on healthcare expenses. A study from Johns Hopkins found that home hospitalization cost roughly 32% less than traditional hospital care (an average difference of $5,081 vs. $7,480 for applicable hospitalizations). However, other studies have failed to show any significant difference in the average costs of home hospitalization vs. inpatient care. One might also worry about many possible unintended and unwanted consequences of a program such as this. For example, if it becomes easier for busy ED physicians to simply clear out patients by sending them back home under this program, you might find that the home hospitalization program becomes inappropriately overused, ultimately driving CMS costs up instead of down. The program might also be abused from the consumer side, where individuals seek out the comfort and/or benefits of this service inappropriately. Again, driving total costs up instead of down. However, for the time being, it is a potentially promising program that will undoubtedly need further tweaking as it matures.
If you or a loved one is facing a possible hospitalization --or are/is currently hospitalized-- consider asking your physician if their hospital is participating in a home hospitalization program and whether that is a suitable option for your treatment.
Sources:
Syphilis is primarily a sexually transmitted disease caused by the bacterium Treponema pallidum (because syphilis is in the genus Treponema, it can also be called a “treponemal disease”; however, there are other treponemal diseases that are not syphilis). It is transmitted through the mucous membranes, broken skin, and direct mother-to-child infection during pregnancy. As such, unprotected sex (anal, oral, vaginal, or any other permutation that results in the exchange of bodily fluids) increases an individual's risk of contracting the disease. Similarly, risky sexual behavior and increased number of sexual partners also increase an individual’s risk of contracting syphilis (and other sexually transmitted diseases).
Syphilis typically presents in three distinct symptomatic stages, (described below) marked by potentially long periods of symptom-free remission between stages. If left untreated, the final stage is usually ultimately fatal. However, it can take up to several decades from the point of initial infection until an individual enters the third and final phase of the disease.
As mentioned above, syphilis commonly presents with three distinct symptomatic stages. These are commonly known as Primary, Secondary, and Tertiary syphilis. Each stage is marked by its own set of typical signs and symptoms of the underlying disease.
● Primary Syphilis usually presents as a single round, painless, firm lesion called a chancre. It usually appears around the genitals or anus, but can occur elsewhere on the body. It usually appears within three weeks of the time of the initial infection. Even if left untreated, the chancre will usually heal within three to ten days.
● Secondary Syphilis usually presents as a more diffuse non-itchy rash across the skin. One of the distinct features of secondary syphilis is that this rash often can involve both the palms of the hands and the soles of the feet. Even if left untreated, this phase will also usually resolve on its own.
● Tertiary Syphilis may occur multiple decades after the initial infection, if left untreated. It can cause diffuse damage throughout the individual’s body to multiple different organ systems, from bone to skin and so forth. However, what often ends up claiming the lives of the afflicted individuals is the damage done to their brain and cardiovascular system. If there is clinical suspicion of syphilis, the individual will still require additional laboratory testing to confirm the diagnosis.
Individuals infected with syphilis can still be accurately tested even if they do not have any active symptoms suggestive of syphilis. This is done by a combination of two blood tests:
1. A nontreponemal test, such as the Venereal Disease Research Laboratory (VDRL) or Rapid Plasma Reagin (RPR) test.
2. A treponemal test, such as the Treponema pallidum Passive Particle Agglutination assay (TP-PA), Enzyme Immunoassays (EIA), Chemiluminescence Immunoassays (CIA), or rapid treponemal assays.
A positive result for both the nontreponemal and treponemal tests is required for a diagnosis of syphilis. Additionally, if there is access to drainage or fluid from an open lesion, urinary discharge, or the tissue from a lesion, darkfield microscopy can be used to look for visual confirmation of the presence of Treponema pallidum (which appear as little white spirals under the microscope, hence their alternate classification as a “spirochete” bacteria).
As dismal and dire as untreated syphilis is, the good news is that syphilis is easily treatable and curable if caught before entering the tertiary syphilis stage of the disease. The mainstay of treatment is an injection of a long-acting form of penicillin called benzathine penicillin G. Because syphilis can be transmitted directly from mother to child during pregnancy, treatment with benzathine penicillin G is highly recommended for infected pregnant women to prevent congenital syphilis in the child. There is even evidence supporting additional treatment for pregnant women. However, because of the additional risks, this issue should be discussed with the woman’s obstetrician to decide on the best treatment plan and course of action.
Book Appointment Now Call For An Appointment
Both the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) have recently reported drastically increased rates of syphilis and, correspondingly, congenital syphilis recently. The WHO estimates that 7.1 million people globally acquired syphilis in 2020. The table below from the CDC shows a 78.9% increase in syphilis cases generally over the 5-year period from 2018 to 2022. Even more concerning, over that same 5- year period there was a 183.4% increase in congenital syphilis (that is, syphilis transmitted from an infected pregnant woman to her unborn child), and a 937% increase from a decade ago.
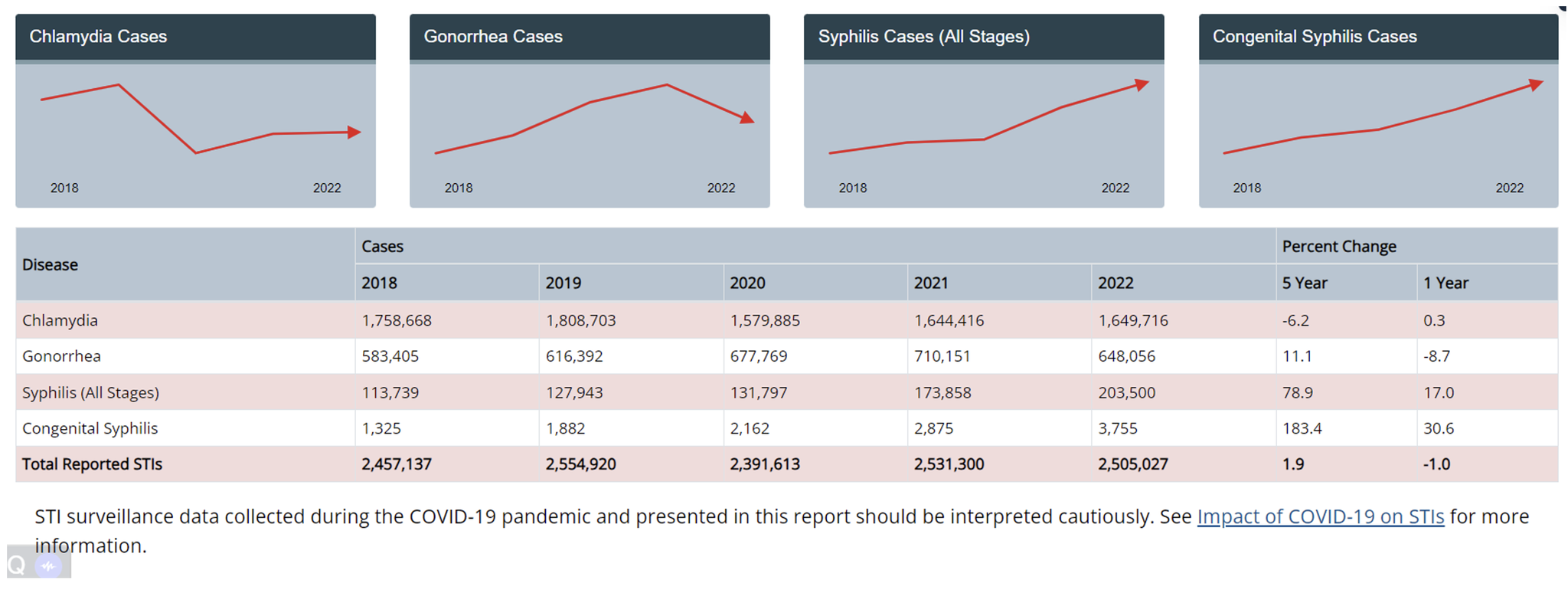
Among the greatest risk factors for syphilis are high risk sexual behaviors and a high number of sexual partners. However, what is surprising about the data is that the incidences of chlamydia and gonorrhea have remained relatively flat over that same 5-year time period. This would seem to suggest that there has not necessarily been an increase in risky sexual behaviors, but rather that the prevalence of syphilis has been increasing within the general population.
There are many potential reasons for this. One of the most commonly cited explanations by health organizations is insufficient testing for syphilis. One much less credible explanation given is a shortage of long-acting penicillin (trade name Bicillin) over the past year. While that might explain a rise over the past year, it does little to explain the rising trend over the 10 years prior. Moreover, there are other alternative treatments for syphilis, such as doxycycline.
One thing that is important to know about the disease course of syphilis is that it often has long periods where the infected individual may have no symptoms at all, and these periods can be up to decades long! Consequently, infected individuals who are asymptomatic are less likely to seek medical attention for testing and treatment. This, in turn, means that infected individuals could potentially be unwittingly transmitting the disease to others for years at a time before their syphilis symptoms recur and prompt seeking medical treatment. Syphilis is further complicated
by the fact that it can present in all manner of symptoms that one might not necessarily associate with a classic STD, thus leading to failure to successfully recognize and treat it. For this very reason syphilis is often colloquially called “the great imitator” amongst the medical community.
Greater awareness amongst both the general population and medical providers, combined with developing better and more frequent testing protocols would likely go a long way towards stemming the rising tide of syphilis. Successfully squelching syphilis need not be a Sisyphean task.
Book Appointment Now Call For An Appointment
When we think of sinusitis, common symptoms like nasal congestion, headaches, and facial pain come to mind. However, there's an uncommon symptom that often goes unnoticed - facial numbness. My Virtual Physician recognizes the importance of understanding this lesser-known connection and provides expert guidance on managing sinusitis effectively.
Sinusitis, an inflammation of the sinuses, typically brings discomfort around the nasal area. But can it cause numbness in the face? Indeed, in some cases, the inflammation and swelling can put pressure on facial nerves, leading to a sensation of numbness or tingling. This phenomenon is not widely known, and many may not immediately associate it with sinusitis. Understanding this link is crucial, as facial numbness can be alarming. It's a sign that sinusitis might be more severe or complicated than usual. My Virtual Physician emphasizes the importance of not dismissing such symptoms and seeking professional advice for a proper diagnosis.
Self-diagnosis can be risky, especially with symptoms like facial numbness. It's essential to consult healthcare professionals like those at My Virtual Physician. They can determine whether the numbness is indeed related to sinusitis or if it's a sign of another underlying condition. Sinusitis, especially when severe, can lead to complications if not treated appropriately. A professional diagnosis ensures that you receive the right treatment, preventing the condition from worsening or leading to further health issues.
In today's digital age, accessing healthcare has become more convenient through telemedicine services like My Virtual Physician. Consulting online for symptoms like facial numbness due to sinusitis not only saves time but also provides access to specialized care right from your home. My Virtual Physician offers comprehensive care for sinusitis, including understanding and managing unusual symptoms like facial numbness. Their expertise in telemedicine ensures that patients receive prompt and accurate diagnoses, followed by effective treatment plans.
If you're experiencing facial numbness along with other sinusitis symptoms, it's time to consult a physician. My Virtual Physician advises not to wait until symptoms become unbearable. Early consultation can lead to a quicker diagnosis and treatment, preventing the progression of the condition. Sinusitis with symptoms like facial numbness might require more than just over-the-counter medication. It's a sign that your body is reacting more intensely to the inflammation, and professional medical advice is crucial in such cases. Understanding Sinusitis in the Digital Age The rise of telemedicine has made managing health conditions like sinusitis more accessible. My Virtual Physician stands at the forefront, providing expert medical consultations online. For anyone experiencing sinusitis symptoms, especially something as unusual as facial numbness, My Virtual Physician offers a convenient and reliable solution. Remember, understanding your symptoms is the first step toward effective treatment. Don’t hesitate to reach out to My Virtual Physician for personalized advice and comprehensive care for your sinusitis concerns.
If you're experiencing symptoms of sinusitis, particularly facial numbness, consider booking an appointment with My Virtual Physician. Their team of experienced healthcare professionals is ready to provide you with personalized advice and comprehensive treatment options, all from the comfort of your home.
Sinusitis is more than just congestion and headaches. When it presents with a symptom like facial numbness, it's a sign to take action. My Virtual Physician is here to help you understand these symptoms and provide the care you need through convenient telemedicine services. Don't let sinusitis and its unusual symptoms go unchecked. Reach out to My Virtual Physician for expert care tailored to your needs.
In an era where women's health and comfort are prioritized, the Caya Diaphragm emerges as a significant advancement in contraceptive choices. It's not just about preventing pregnancy; it's about embracing a method that aligns with your lifestyle and well-being. My Virtual Physician recognizes this need and stands ready to guide you through understanding how the Caya Diaphragm can be a game-changer in your sexual health journey.
The design of the Caya Diaphragm is a testament to modern medical ingenuity. Its contoured, silicone-based structure is tailored to fit the female anatomy comfortably. This means no rigid edges or uncomfortable fits – just a natural, almost unnoticeable presence during use. For women who have experienced discomfort with other contraceptive methods, the Caya Diaphragm offers a breath of fresh air. Its material is hypoallergenic, making it suitable for women with sensitivities or allergies to latex.
Moreover, the comfort it provides goes beyond the physical aspect. There’s a mental ease that comes from using a product that’s designed with your body in mind. This can significantly impact your sexual health positively, making intimate moments more enjoyable without the worry of discomfort.
When it comes to contraception, effectiveness is a non-negotiable. The Caya Diaphragm, backed by clinical research, offers impressive reliability. Its design is such that, when used correctly and with spermicide, it forms a physical barrier that prevents sperm from reaching the uterus. This method’s success rate is encouraging, giving women confidence in their contraceptive choice.
It's important to note that the effectiveness of any contraceptive method, including the Caya Diaphragm, depends on proper use. This is where My Virtual Physician comes into play. Our team is dedicated to educating you on the correct usage, ensuring that you get the most out of your Caya Diaphragm.
Choosing a contraceptive method that you're comfortable with can have a profound effect on your sexual well- being and relationship satisfaction. A method that is both comfortable and reliable like the Caya Diaphragm can reduce anxiety around intercourse, leading to a more fulfilling sexual experience. This peace of mind is invaluable, allowing you to focus on the intimacy and connection with your partner.
Furthermore, the Caya Diaphragm does not interfere with the body’s natural hormonal balance. This is a crucial factor for many women who prefer or need to avoid hormonal contraception for various health reasons.
My Virtual Physician’s commitment to empowering women with choices is evident in our support for the Caya Diaphragm. We understand that each woman’s needs are unique, and our approach is to provide personalized consultations. Through telemedicine, access to this modern contraceptive method is simplified, making it a viable option for women everywhere.
Our platform provides not just access but also comprehensive education about the Caya Diaphragm. We believe in informed choices, and our team ensures that you have all the information you need to make the best decision for your health and lifestyle.
The Caya Diaphragm represents more than just a contraceptive method; it's a statement of comfort, reliability, and empowerment. My Virtual Physician is here to help you explore this option, ensuring that your journey in sexual health is supported, informed, and aligned with your personal values. We invite you to schedule an appointment with us for a personalized consultation on using the Caya Diaphragm and to address any sexual health concerns you may have. Remember, your comfort and health are paramount, and with the Caya Diaphragm, you’re choosing a path that respects both.
When it comes to choosing medications, one of the most common dilemmas people face is deciding between generic and brand-name drugs. At My Virtual Physician, we understand the importance of making informed health decisions. That's why we're delving into this topic to clear up misconceptions and provide you with the knowledge you need.
One might wonder, "Are generic medications the same as brand names in terms of quality and effectiveness?" The answer is a resounding yes. Generic drugs are equivalent to their brand-name counterparts in the most crucial aspects - safety, efficacy, and therapeutic value.
Generic medications undergo rigorous testing and approval processes. The U.S. Food and Drug Administration (FDA) requires that generics demonstrate bioequivalence to brand-name drugs. This means they must have the same active ingredient, strength, dosage form, and route of administration. The manufacturing facilities and processes also meet the same high standards as those of brand-name drugs.
The primary difference between generic and brand-name drugs lies not in their quality but in their accessibility. Generics offer significant economic benefits. They are typically far more affordable than their branded counterparts, making essential medications accessible to a broader range of people. This cost-effectiveness can be a game-changer, especially for individuals managing chronic conditions on a budget.
Despite their proven efficacy, some myths persist around generic medications. A common misconception is that cheaper means lower quality. However, the lower price of generics is due to the absence of the initial research, development, and marketing costs that brand names incur. The quality, safety, and effectiveness remain on par with branded drugs.
At My Virtual Physician, we emphasize personalized healthcare. Understanding your medication options, including the viable choice of generics, is a crucial part of this. We encourage patients to discuss their medication options with our healthcare providers, ensuring they make choices that best suit their health needs and financial circumstances.
In the end, generic medications are not just a cost-effective alternative; they are a safe, effective, and essential part of modern healthcare. By choosing generics, patients can access the treatments they need without compromising on quality.
We encourage our readers to continue exploring these topics. If you're considering switching to generic medications or have any questions about your medication choices, we invite you to schedule a consultation with My Virtual Physician. Our experts are here to provide personalized advice and support your journey towards informed health decisions.
Remember, your health is your most valuable asset. Making educated choices about your medications is a critical step in managing it wisely. At My Virtual Physician, we're committed to guiding you through these choices, ensuring you receive the best possible care tailored to your unique needs.
In the world of healthcare, trust and care form the cornerstone of a strong patient-doctor relationship. With the advent of telemedicine, this dynamic is evolving. My Virtual Physician, a leading online primary care provider, is at the forefront of this evolution, demonstrating how trust and care can flourish even in the digital healthcare landscape. This article explores the importance of these elements in an online setting and how My Virtual Physician is setting a new standard for patient care.
In traditional healthcare settings, trust is built over time through face-to-face interactions. However, in the digital world, building trust with an online primary doctor requires a different approach. My Virtual Physician understands this and has crafted a platform that fosters trust from the first interaction. The use of secure, user-friendly technology for consultations ensures that patients feel safe sharing their health concerns. Moreover, the consistent quality of care and attention to detail in follow-ups reinforces this trust, proving that distance is no barrier to a reliable healthcare relationship.
My Virtual Physician’s commitment to confidentiality and adherence to medical ethics further enhances this trust. Understanding that patients might have concerns about data security and privacy, the platform uses state-of-the- art security measures. This commitment ensures that the sanctity of the patient-doctor relationship is maintained, just as it would be in a traditional setting.
The key to a strong patient-doctor relationship lies in understanding and empathy. My Virtual Physician’s team of dedicated doctors takes the time to understand each patient's unique health journey. Through regular virtual check-ins and personalized health plans, patients receive care that is tailored to their individual needs. This personalized approach not only addresses the immediate health concerns but also fosters a sense of belonging and care, vital for long-term health management.
Telemedicine’s flexibility allows for more frequent and convenient communication between patients and doctors. This regular interaction builds a deeper understanding and a stronger bond, akin to what one would expect from a traditional family doctor. My Virtual Physician leverages this advantage, ensuring that patients always have access to their doctors, whether for acute conditions, chronic disease management, or preventive care.
Access to a reliable online primary doctor means healthcare on your terms – flexible, accessible, and tailored to your lifestyle. For busy professionals, parents juggling family responsibilities, or individuals in remote areas, My Virtual Physician provides a level of accessibility that traditional healthcare often cannot match. This ease of access ensures that health concerns are addressed promptly, leading to better health outcomes.
Moreover, the continuity of care provided by online primary doctors is invaluable, especially for managing chronic conditions. Patients have the assurance of consistent care from a doctor who understands their medical history in- depth, an aspect often missing in fragmented traditional care models.
Patient testimonials and case studies are a testament to the successful relationships built through My Virtual Physician. From managing chronic illnesses to providing acute care and preventive advice, these stories reflect the positive impact of having a trustworthy online primary doctor. These real-life examples highlight how an empathetic, patient-centric approach, combined with the convenience of online consultations, can lead to meaningful and long-lasting healthcare relationships.
Take the Next Step
My Virtual Physician is more than just a platform for healthcare; it’s a community where trust, care, and professional medical advice converge to provide a holistic online healthcare experience. For those new to telemedicine or seeking a more connected healthcare journey, My Virtual Physician offers an opportunity to experience healthcare reimagined.
Ready to experience a new level of healthcare? Visit myvirtualphysician.com to learn more about our services and book your initial consultation. Discover the difference of a patient-doctor relationship that’s rooted in trust and care, all from the comfort of your home.
In recent years, the United States has witnessed an unsettling surge in cases of newborn syphilis, reaching levels not seen in the past three decades. According to the latest data from the Centers for Disease Control and Prevention (CDC), there has been a tenfold increase in newborn syphilis cases over the last decade, with more than 3,700 infants born with the infection in 2022 alone. Federal health officials are raising the alarm, emphasizing the urgent need for action to curb this concerning trend.
Syphilis, a sexually transmitted infection caused by the bacterium Treponema pallidum, can be transmitted from an infected mother to her unborn child, leading to congenital syphilis. The consequences of untreated syphilis in newborns can be severe, ranging from developmental issues to organ damage and even death. The rise in cases is a stark reminder of the importance of timely and accessible healthcare, especially for expectant mothers.
Amidst the alarming statistics, there is hope for a solution that is both convenient and effective: virtual primary doctor visits and online consultations. My Virtual Physician, a leading telemedicine service, offers a swift and secure way for individuals to address their health concerns, including the need for syphilis testing.
My Virtual Physician provides easy access to virtual primary doctor visits, allowing individuals to consult with healthcare professionals from the comfort of their homes. This eliminates barriers such as transportation issues or the need for childcare, making healthcare more accessible to everyone.
With My Virtual Physician, patients can receive electronic lab orders that are seamlessly sent to the nearest laboratory of their choice. This streamlined process ensures that individuals can get tested for syphilis promptly, without the need for additional paperwork or physical visits.
In addition to syphilis, My Virtual Physician offers comprehensive STD testing, including screening for HIV, hepatitis C, HSV, gonorrhea, and chlamydia. This holistic approach allows individuals to address multiple health concerns in a single telemedicine visit, promoting overall well-being.
As the nation grapples with the rising tide of newborn syphilis cases, it is crucial to embrace innovative solutions that can make healthcare more accessible and efficient. My Virtual Physician stands as a beacon of hope, offering a convenient avenue for individuals to address their health concerns promptly and responsibly. Through quick telemedicine visits and electronic lab orders, this service plays a pivotal role in the fight against syphilis and other sexually transmitted infections, ensuring a healthier future for all.
Don't wait – take control of your health today with My Virtual Physician and contribute to the collective effort to combat the alarming rise of newborn syphilis in the U.S.
Telemedicine practices are on the rise, revolutionizing the way healthcare is delivered. However, a recent survey reveals that 55% of physicians find a misalignment between their patients’ expectations and what can be achieved through a virtual care model.
My Virtual Physician (MVP) stands out as an innovator, sharing the belief that virtual care can accomplish more for patients than ever before. While some providers offer a hybrid care model combining virtual and in-person visits, a hybrid model alone may not provide comprehensive care.
Let’s compare My Virtual Physician against Doctor on Demand, another popular telehealth provider, to see where MVP is breaking barriers in virtual healthcare.
Doctor on Demand is an established telemedicine provider offering virtual visits to treat specific conditions for patients. While they offer some primary care services, their scope of services is limited. Here’s a side-by-side comparison of treatment options:
| My Virtual Physician | Doctor on Demand | |
| Allergies | ✔️ | ✔️ |
| Earaches | ✔️ | ❌ |
| Cough, Cold, & Flu | ✔️ | ✔️ |
| Sinus Infection | ✔️ | ✔️ |
| Skin Rashes | ✔️ | ✔️ |
| Pediatric Care | ✔️ | ✔️ |
| Perinatal Care | ✔️ | ❌ |
| STD | ✔️ | ✔️ |
| Women’s Health | ✔️ | ✔️ |
| Irregular Periods | ✔️ | ❌ |
| Painful Periods | ✔️ | ❌ |
| Birth Control | ✔️ | ❌ |
| Infertility | ✔️ | ❌ |
| Menopause | ✔️ | ❌ |
| Acne | ✔️ | ✔️ |
| Mobile Testing | ✔️ | ❌ |
| Medical Marijuana | ✔️ | ❌ |
| Mental Health | ✔️ | ✔️ |
| Specialty Care | ✔️ | ❌ |
| Wound Care | ✔️ | ❌ |
| Chronic Condition Management | ✔️ | ❌ |
Doctor on Demand and My Virtual Physician are both complete care providers offering patients access to urgent care, primary care physicians, and pediatricians for online doctor appointments.
Another similarity between the two virtual providers is the availability of virtual and in-person visits. Doctor on Demand partners with certain facilities and helps patients find physical care providers.
My Virtual Physician, on the other hand, owns two clinics in Las Vegas with a care team employed on-site. They also provide virtual doctor visits to all 50 states offering a range from primary to specialty care physicians.
Doctor on Demand and My Virtual Physician appear to go toe-to-toe on paper until you start reading the fine print. That’s where MVP stands apart. My Virtual Physician is staffed with specialists, including:
And they are working to add even more specialist physicians for patients to have direct access to specialized care without a referral.
As far as pricing goes, Doctor on Demand comes with a bit of sticker shock. For a 15-minute virtual consultation for primary care, patients can expect to pay $79, while a 45-minute consultation with a Psychiatrist is nearly $300.
My Virtual Physician offers patients greater flexibility and a more straightforward pricing model. Visits are broken down into categories of acute, comprehensive, and specialty care. Depending on the nature of your visit, you’ll pay:
Reviews and ratings of telemedicine platforms provide valuable insights into patients’ experiences. Let’s address the elephant in the room between these two platforms. Doctor on Demand has a 1.5 rating on Trustpilot, indicating a significant number of negative experiences reported by users. Common complaints mention:
On the other hand, My Virtual Physician stands in stark contrast, boasting over 100 5-star reviews on Google. These positive ratings signify high satisfaction and appreciation from patients who have received care.
My Virtual Physician is no doubt the forerunner in revolutionizing healthcare through telemedicine, particularly for those in remote situations. They provide a total care approach for individuals with multiple chronic illnesses, using mobile teams of certified medical assistants (MA) and specialty physicians including OBGYNs, pediatricians, internists, and more.
This mobile team coordinates evaluations and consultations using an actual hybrid approach, where a medical assistant travels to the patient’s home with a tablet for video connections with doctors. The MA uses assistive technology to perform physical tasks such as:
Through the power of telemedicine, doctors can directly observe and supervise critical treatments, such as wound care, from the comfort of the patient’s own home. This convenient and inclusive approach breaks barriers ensuring individuals receive comprehensive care and specialized treatments regardless of their circumstances.
Doctor on Demand and My Virtual Physician both offer online telemedicine services, providing a range of treatment options and accessible healthcare services.
While Doctor on Demand caters to non-emergency medical conditions, mental health concerns, and general medical advice, My Virtual Physician takes it a step further by offering a more extensive and specialized approach to care.
The best thing about telemedicine is that patients can reach more providers now than ever possible before. This gives patients the power to choose from more than one provider for their healthcare needs. If you’re ready to check out what My Virtual Physician can do for you, our doctors are standing by to help.
Book Appointment Now Call For An Appointment
The human body miraculously knows just what to do and when to do it.
Your heart beats on its own, your lungs draw in air and push out carbon dioxide without any intentional effort on your behalf, and your food goes through your body, nutrients absorbed, and waste removed without much conscious instruction.
But sometimes, those bodily processes can get out of whack. When there is pain or disruption in automatic functioning like swallowing and digestion, it grabs our attention. Luckily, today’s technology allows doctors to see what’s happening inside the body without the use of a scalpel.
In this blog, we’ll talk about one way to look inside the body called an EGD. Find out:
EGD (esophagogastroduodenoscopy) is a medical procedure used to examine your esophagus, stomach, and part of the small intestine (duodenum). During an EGD, a special tool called an endoscope is used to examine the upper GI tract. An endoscope is a soft, flexible tube with a camera attached to the end.
At the start of the EGD procedure, the endoscope enters the body through the mouth for visual inspection of the upper GI tract. This helps doctors identify any ulcers, irritation, or bleeding that may be the cause of your discomfort. Some endoscopes are even equipped with accessories for collecting biopsies (tissue samples) so that they can be sent to the lab for further analysis.
An EGD can also double as a treatment for some upper GI concerns. Some endoscopes are capable of cauterizing bleeds or removing polyps (small growths) during the procedure.
Since an EGD is a diagnostic procedure, you only need it if you’re having symptoms of an illness in the upper digestive tract. Here are some common problems that warrant a closer look through EGD:
Your doctor will help determine whether an EGD is necessary to diagnose the cause of your discomfort. If you’re experiencing the above symptoms or struggling to manage a digestive condition, My Virtual Physician can help. Reach out to our doctors today for a virtual appointment.
If you’re already scheduled for an EGD, you may be wondering what the experience will be like. We’ll cover that next.
It sounds pretty uncomfortable to have someone poking around inside you with a tube down your throat during the EGD procedure. Luckily, you will be under mild sedation as an outpatient procedure, allowing your experience to be very relaxed and pleasant (but still awake).
Before coming in for your EGD, your doctor will provide instructions to prep for the procedure. It’s very important to avoid eating or drinking before your procedure so that you do not aspirate. Aspiration is when your stomach contents are inhaled into your lungs. Aspiration can lead to very serious health problems like pneumonia or even death.
When you arrive at the clinic or hospital for your EG, here’s what will go down:
If you want to learn more about the endoscopy from a doctor’s perspective while you’re in the procedure room zoned out, check out our Talk Tuesday episode below on EGD:
Immediately after your EGD, you should closely monitor your body for signs of infection, bleeding, or perforation. Since an EGD has an inherent risk of serious complications if the endoscope perforates your upper GI tract, it’s critical to go to the ER (or at least speak with a doctor) if you have any of these serious symptoms after the procedure:
About two weeks after your EGD, you’ll have a follow-up appointment with your doctor to go over the findings. If any biopsies were taken, you’ll get results during your follow-up appointment or sooner. In some cases, your doctor may have been able to treat the cause of your symptoms from the EGD alone. If not, your doctor will make recommendations on the next steps required to restore your health.
If you’re struggling with digestive issues, talk to a specialist at My Virtual Physician for help. Our virtual appointments are easy, affordable, and convenient. And our team of doctors is passionate about helping you get well. We can help you decide whether an EGD is the best route to take or if there are alternative solutions to try first.
 Everyone needs to see a doctor at some point in their lives. Whether you’re facing an illness, pain, disorder, or just need a medication refill or regular checkup; our society relies heavily upon primary care physicians.
Everyone needs to see a doctor at some point in their lives. Whether you’re facing an illness, pain, disorder, or just need a medication refill or regular checkup; our society relies heavily upon primary care physicians.
How long has it been since you last saw yours?
It can be a struggle to get an appointment scheduled with your Las Vegas primary care physician (PCP). Waits are long and many doctors aren’t even accepting new patients. One reason for this is that there is a shortage of physicians.
Related: Increasing Access in Las Vegas: Physician-to-Patient Ratio
That may leave you wondering—what can I do to see a Las Vegas doctor sooner? Read on to find out a solution to the doctor access dilemma.
Availability isn’t the only problem that patients face when trying to schedule doctor appointments in Las Vegas. Physical limitations, such as transportation, access to technology, and geographical location, can also hinder access for patients to see their doctors regularly.
A primary care physician, or PCP for short, is a general practitioner who you know as your “go-to” doctor. Any time you have an infection, need medication, or want a consultation, your PCP is probably your initial point of contact.
This type of doctor sees a broad range of patients, in the age ranges of anywhere from children to the elderly, and treats a wide variety of conditions. If you have to manage an ongoing health condition, such as diabetes or asthma, you likely see your PCP more frequently.
While it’s not necessarily required to have a PCP, establishing a relationship with a primary care doctor in Las Vegas can be beneficial for both patients and physicians. That’s because your doctor can get to know you, your health, and you become comfortable with one another to discuss private health matters.
Here’s a list of common conditions or patient needs that most primary care physicians are capable of handling without the need for specialist visits:
But if you can’t get in to see your PCP or get established with a new primary care doctor in Las Vegas, then what can you do?
My Virtual Physician has a new solution to the patient access problem in Las Vegas. Our Las Vegas specialists can provide PCP services online through our hybrid clinic on Paradise Road.
Related: Hybrid Medical Clinics: Expanding OBGYN Access in Las Vegas
This physical clinic solves many problems when it comes to patient access to doctors in Las Vegas.
Can’t get an appointment? No problem, walk-in visits are welcome in our hybrid clinic.
No computer, phone, or internet connection? Our hybrid clinic offers a private room with all the technology already set up for our patients to use.
Need a second opinion? Our professional doctors are available to meet with you today to provide medical advice.
Uninsured? My Virtual Physician offers affordable and transparent pricing on our telemedicine appointments, both in the clinic and online.
Stop waiting for an opening at your traditional doctor’s office. See a doctor today in Las Vegas who can meet your healthcare needs.
Book Appointment Now Call For An Appointment
Need to see a specialist? Whether you’re looking for a Las Vegas OBGYN or a pediatrician for your child, getting established with a specialist physician can be an intimidating venture.
It used to be a lengthy, expensive, and convoluted process.
Luckily—things have changed. Today, there’s a new path available for patients. Now, you can see a healthcare specialist without the red tape.
More providers are paying attention to the patient experience, and a clear demand has surfaced: patients need easier access to specialists for healthcare. Healthcare specialist appointments must be easily accessible, swiftly scheduled, and transparently priced.
In this blog, we’ll define what specialists are and when you need to see them. And then, we’ll explore the processes required to see a healthcare specialist, both old and new—letting you in on the secret to seeing a Las Vegas Specialist in a snap.
When you call to schedule your appointment for your annual physical or a routine checkup, you’re likely booking with your primary care physician. These doctors can handle a wide range of common medical ailments seen in the general population.
A specialist, on the other hand, is a doctor who has expertise in a particular body system.
For example, an OBGYN specializes in the female reproductive system. Read more about the special care focus of an OBGYN below in the related blog at the link below.
Related: What’s an OBGYN: Get to Know Our Las Vegas Gynecology Team
An ENT doctor specializes in ailments of the ears, nose, and throat. A pediatrician specializes in the healthcare needs of children.
Here are some other specialists found in our healthcare system:
This is just a small selection of the many specialty fields out there in the world of healthcare.

There are many reasons to seek medical care from a healthcare specialist. Here are a few.
If you’re experiencing a chronic medical condition that your primary care doctor is unable to treat, it may be time to see a specialist. For example, if you’ve been asking your regular doctor to help clear up a skin condition, but it doesn’t seem to be improving—a dermatologist, who specializes in skin conditions, may be more qualified to help. Sometimes your doctor will refer you to a specialist; other times, you may need to seek out the specialist yourself.
Primary care physicians (PCPs) are trained to treat a broad scope of conditions that occur in the general population. If you know that you have a condition that is rare or that a specialist is more qualified to treat, then it may be appropriate to book directly with a specialist rather than a PCP. For example, if you have irregular menstrual cycles, an OBGYN or endocrinologist may be better able to pinpoint a care plan than a doctor with general training.
A third reason that patients desire to see a specialist is to find a doctor who is more familiar with treatment options that they have researched. If a primary care doctor is unfamiliar with a treatment that you want to try, seeing a specialist with experience using the treatment is a valid option.
So, now that you know when it’s time to see a specialist—let’s look at how to do it.
First, the long way.
Traditionally, the process of seeing a specialist involved making multiple appointments. Ultimately, your primary care physician was the gatekeeper who decided whether patients were permitted to schedule an appointment with a specialist.
Sometimes, you’d also need to have pre-approval from your insurance company before seeing a specialist. Insurance companies may deny coverage of specialist visits if the proper referral paperwork is not filed by your doctor’s office.
With the traditional method, you had to jump through hoops to see a specialist physician, including:
With the shortage of specialists in the Las Vegas area, seeing an OBGYN or other specialists in the area could take months.
Luckily, there’s a better way!
It’s hard to believe that anyone would follow the long process above to see a healthcare specialist when there’s such a simple shortcut. So, how can you see a specialist physician without jumping through hoops?
Schedule directly with your specialist.
My Virtual Physician wants patients to have access to specialists. That’s why we are here. Our patients have the option to visit with our Las Vegas specialists either online or inside our hybrid clinic located on Paradise Road in Las Vegas.
Our specialists include:
My Virtual physician offers transparent pricing and affordable visits for self-paying patients. Read more about grabbing affordable medications as a self-pay patient below.
Related: Guide to Self-Pay Prescriptions: Get the Best Price on Medications
If you’re located or visiting the Las Vegas area, walk-ins are welcome at our hybrid clinic. At this clinic, you can visit virtually with our specialists inside a private exam room right on the Vegas strip, making seeing a specialist on your own terms as easy as can be.
If you’re ready to book your appointment with one of our specialists, click below to self-schedule or walk into our hybrid clinic for an instant appointment. We look forward to serving you by providing a positive patient experience.
Book Appointment Now Call For An Appointment
You’ve been planning this vacation for months and now you’ve arrived—you finally made it to Vegas! Now, the fun begins…
You’re full of excitement and ready to experience the Vegas strip and have some fun! But there’s one detail that you probably didn’t plan out while you were booking tickets, packing your bags, and making your way to Nevada.
That detail is this—what to do if you need to see a doctor while you’re on vacation.
If you’re insured, seeing an out-of-state doctor may mean that you’ll face steep out-of-network charges that don’t count toward your regular deductible. If you’re uninsured, you might get stuck with hefty out-of-state medical bills.
If you’ve just arrived at your hotel in Las Vegas and realized you need to see a doctor ASAP, here’s what to do in order to see a doctor quickly and affordably so that you can turn your focus back to enjoying your vacation.
Before making any decisions, just pause for a moment. Focus on the reason that you need to see the doctor. If it’s because you forgot your medications at home, then write down the medications that you need refilled in Las Vegas to cover you during your vacation.
On the other hand, if you’re having indications of an illness that requires medication for you to feel better, write down your symptoms and how long you’ve had them. Some common illnesses that pop up during vacation include UTIs and bacterial infections.
If you feel a urinary tract infection (UTI) coming on or you are experiencing a sudden and extreme sore throat, write down your answers to the following questions:
In many cases, you’ll continue to feel miserable until you get antibiotics to fight the infection if it’s caused by bacteria. Tracking your symptoms as soon as you notice them can help you evaluate whether things are getting worse.
Related: What To Do If You Are Traveling With a UTI on Your Road Trip to Las Vegas
Take an account of the facts and assess the urgency of your situation before reacting. Once you’ve got your troubles documented, you can make an informed decision on whether or not you need to see a doctor.
The next step before taking action is to figure out the best type of doctor that can help you. A general practitioner can handle many common health concerns. But local doctors probably won’t have an opening for months and an urgent-care clinic staffed with general practitioners might cost you a small fortune in medical bills.
If your medical need requires a specialist, how can you find one in Vegas? Specifically, can you find an OBGYN in Las Vegas? OBGYNs specialize in the female reproductive system and cover anything from contraceptive prescriptions to menstrual problems and infertility. Read more about what conditions OBGYNs treat.
Once you’ve narrowed down whether it’s a general practitioner or a specialist that you need to see, you can start looking for a doctor or clinic. The two main places to look are in-person clinics in Las Vegas or online.
Telemedicine has provided greater access to healthcare and specifically, to specialists. Today, you can see a doctor in minutes rather than months. Searching for a provider online (who is licensed to practice in Nevada) can be one of the simplest solutions to finding a provider while traveling.
Online providers also tend to be more self-pay friendly. Since insurance companies don’t typically cover out-of-network providers, going online can be an affordable alternative. You’ll find a wide selection of specialists online who are taking new appointments.
Related: What to Expect During an online OBGYN Las Vegas Appointment
If you prefer a brick and mortar visit to the doctor without breaking the bank, My Virtual Physician has created a hybrid clinic to meet that need. Located on Paradise Road in Las Vegas, this clinic offers televisits for walk-ins and same-day appointments. Appointments are available for a flat, affordable price. Get back to the fun after stopping by the hybrid clinic on Paradise Road.
Our hybrid clinic is staffed virtually with a variety of physicians and specialists (including pediatricians and OBGYNs) to help you get feeling better faster.
If you’ve been prescribed medication during your hybrid or telemedicine visit, picking it up is also a simple process. You’ll need to find a Las Vegas pharmacy that is nearby so that you can get your prescription right away. There are several pharmacies within walking distance of our hybrid clinic where your doctor can send your prescription to be filled.
For help finding the most affordable local pharmacy, check out our guide to self-pay prescriptions below.
Related: Guide to Self-Pay Prescriptions: Get the Best Price on Medications
My Virtual Physician is proud to provide greater access to doctors and specialists, particularly in the Las Vegas area with our hybrid clinic on Paradise Road. Our board-certified Las Vegas team of OBGYNs, pediatricians, and other specialists are here to help if you find yourself needing to see a doctor urgently while on vacation in Las Vegas or elsewhere.
Walk into our hybrid clinic today or schedule your online appointment now by clicking below.
Book Appointment Now Call For An Appointment
Holiday traditions encourage families to get together to celebrate with distant relatives—including aunts, uncles, grandparents, and in-laws. This is an opportunity to catch up with one another and find out how everyone in your family has been doing since you were last together.
Family get-togethers are also a suitable occasion to recognize when something isn’t quite right. This season provides a short window of opportunity for intervention when someone is crying out for help from elder abuse.
In this article, we aim to spread awareness about elder abuse during this holiday season by covering:
Elder abuse is when a trusted caregiver knowingly or negligently takes advantage of an elder—it can include physical or sexual abuse—or take another form, such as:
The elderly tend to be more vulnerable to abuse than other adults. That’s because there is a gradual decline in physical strength and mental acuity as we age. Many of our elders also depend on caregivers to help with day-to-day functioning.
According to the American College of Obstetricians and Gynecologists, as many as one in ten adults over the age of 60 may become a victim of elder abuse. And only around 1 in 23 cases of elder abuse are reported to authorities. With such a high incidence, it’s critical to know what to look for to spot elder abuse.
Doctors often screen for signs of elder abuse during regular visits, and the ACOG recommends that OBGYNs screen all patients over the age of 60 for signs of abuse.
But doctors are not the only ones who can recognize the signs of abuse. When you meet with your loved ones this holiday season, look deeper at any red flags that grab your attention.
For example, if your grandpa shows up to Christmas dinner with teeth missing from his dentures and unkempt hair, you might begin to look for other signs that he is not receiving proper care. If your aunt, who takes care of grandpa, has a shiny new car out of the blue and a bad attitude toward grandpa—that’s worth investigating further.
Here are some other signs to look out for:
If you notice any of these signs, it’s worth investigating whether your family member has become a victim of elder abuse. Talking to your loved one directly about the red flags may not be enough to get them the help they need—so what can you do to get real help if you suspect elder abuse?
Our elders deserve protection. If you suspect elder abuse, the best course of action is to report it to authorities, who are trained to investigate this type of situation. You can report suspected abuse to a number of agencies, including:
The National Center on Elder Abuse website has state-specific resources for you to contact the right professionals in order to get help in your region.
If you’re not sure whether your loved one is suffering from abuse, you can encourage your elder to see his or her doctor, who will do an elder abuse screening. Physicians are mandated reporters, which means that they must report suspected abuse to authorities.
Sadly, elder abuse is not an uncommon occurrence. But the good news is that everyone has the ability to do their part to help stop the abuse. Simply reporting any suspicions to the proper authorities may be enough to put an end to elder abuse.
My Virtual Physician prioritizes protecting vulnerable populations and can help with the reporting process. Contact us today if you or a loved one needs help.
Virtual doctors are making waves. Atlanta Medical Center (AMC) in Atlanta, Georgia, has closed its doors to two facilities this year, including the most recently closed downtown location. According to Wellstar, the organization that ran these hospitals, the closures are caused by a lack of revenue, a side effect of rising inflation.
Atlanta isn’t the only community affected by this trend. Even rural hospitals have seen an increase in facility closures. Are virtual doctors the solution or the cause?
Read below to find out how virtual doctors are changing healthcare.
Telemedicine exploded during and after the pandemic. A new way to see your doctor on-screen became the norm. And it stuck. Here are a handful of reasons that virtual doctors are now preferred by patients over in-person visits, leaving hospitals and other in-person medical facilities hanging.
Getting into your doctor for a preventative visit or even to solve a new health problem used to take an excessive amount of time.
First, you had to wait on hold to get an appointment, then you had to wait weeks or months for an opening, then you had to commute to the appointment, and when you finally arrived at your scheduled time—you had to wait a little longer until your doctor was ready to see you. That’s a lot of waiting.
Luckily with the recent developments in telemedicine, most of this waiting process has been completely eliminated. No waiting on hold for scheduling, you can get in the same day to see a doctor, and there’s no commute or waiting room to waste your time with.
Telemedicine solves the dilemma of delayed treatment. Telehealth provides an avenue for patients to be seen by doctors and specialists faster than ever before, which means—patients get faster treatment. Today, conditions get treated before they ever have time to fester into major health concerns that require hospitalization.
It’s safe to say that telemedicine cuts down on the need to hospitalize.
Every patient deserves access to medical care. Relying on the outdated infrastructure of brick-and-mortar buildings to meet the entire nation’s medical needs is no longer feasible. Especially when the technology exists to move certain care needs to the digital realm.
Stepping up to the plate, virtual doctors are here to help ease the demand on physical facilities so that they can serve their populations more effectively.
Telemedicine helps by spreading the load of care needs over a larger pool of providers. When a substantial portion of preventative care visits and other types of appointments that don’t require in-person exams can be transitioned online, it makes healthcare more accessible.
Additionally, virtual doctors open doors for access to patients who are affected by hospital or facility closures in their local communities. Physical distance is no longer an obstacle to overcome when it comes to getting medical care for non-emergency situations.
Related: Telemedicine Improves Access to Prenatal Care, But Can We Improve Access to Telemedicine?
When it comes to answering the question posed at the top of this article, the answer is a little bit of both. While telemedicine certainly shifted patients out of hospitals, that’s not a bad thing. Hospitals can now focus on scaling down operations and focusing only on the emergency needs, such as surgical procedures, while leaving preventative and other simple appointments to virtual doctors.
While telemedicine is certainly not the only cause, it has played a part in the shift away from brick-and-mortar facilities. As far as being the solution to hospital closures, virtual doctors certainly proved their value during the pandemic. Telemedicine is here to stay by popular demand and will become the solution for patients who need to see a provider but have no nearby facility available.
Our virtual doctors serve patients in all 50 states. Whether you need to see a primary care physician or a specialist, we’re here to help. Our mission is to provide access to healthcare. If your community recently experienced a shut down of a medical facility or you’ve heard rumblings of disruption, get established with our online doctors today so that you can always get care when the need arises.
Book Appointment Now Call For An Appointment

Imagine a world where you can’t get in to see your doctor for months or even years. Whether you simply need a prescription refill or help diagnosing and managing a chronic medical condition like diabetes, both can produce scary, or even life-threatening, scenarios.
Now, consider that the United States isn’t that far from this reality. In a 2021 report, the Association of American Medical Colleges (AAMC) predicted that a physician shortage is coming to the US. By 2034, the country will fall short of meeting the appropriate physician-to-patient ratios.
In fact, the AAMC believes that the US will fall between 40,000 to 124,000 doctors short in the next decade or so.
It makes sense that densely-populated areas require more doctors in order to meet healthcare needs. That’s where the physician-to-patient ratio comes in. If you can measure this ratio, it tells you whether you have enough doctors to meet a geographical area’s healthcare needs.
Most states within the USA fall below the ideal physician-to-patient ratio. An ideal number is around 270 physicians per 100,000 people. This equates to about 370 patients per doctor. Many states hover around a rate closer to 200:100,000.
The governmental agency known as the Health Resources & Services Administration (HRSA) works to increase healthcare access to vulnerable populations (geographically isolated, economically or medically vulnerable). Reports are available on their website. These reports show where vulnerable populations are located and where physicians are needed the most.
Nevada has been experiencing a physician shortage for some time. Currently, the state’s ratio remains around 200:100,000. Read more here about the OB/GYN Physician Shortage in Las Vegas.
HRSA reports displaying Health Professional Shortage Areas (HPSA) show regions where there is a shortage of providers. Nevada shows 75 areas with a primary care physician shortage, plus numerous dental and mental health areas where there is a shortage of specialists to serve these populations.
A search on medically underserved areas from HRSA shows 25 regions within the state have underserved areas and populations. Specifically, these areas in Las Vegas are underserved:
It is My Virtual Physician’s mission to provide access to healthcare for men, women, and children. That’s why we offer online telemedicine visits for patients in any US state. This helps break down geographical barriers in order to increase the real physician-to-patient ratio. On top of that, we have taken it a step further with our hybrid clinic located in Las Vegas.
Read about our hybrid clinic’s opening here: My Virtual Physician Celebrates Las Vegas Hybrid Clinic Opening.
This clinic helps to serve populations who may not have access to the digital requirements of telemedicine. We provide a private room that our patients can use to meet virtually with our doctors inside the clinic located at 2217 Paradise Road in Las Vegas.
Additionally, the clinic provides immediate access for all populations. Walk-ins are welcome during business hours. Find out more here. Our doctors can provide primary care needs as well as specialty visits. In addition to our primary care doctors, we also have board-certified OBGYNs and Pediatricians ready to meet with patients.

There’s been a recent spike in positive RSV tests in the Las Vegas region. CDC data shows a jump to over 5% of positive PCR tests that began in September and October.
This spike resembles last year’s Vegas RSV data for September, but preliminary information looks like it might be doubling October’s numbers. So is it cause for concern?
Here’s everything you need to know about RSV if you’re living or staying in Las Vegas.
Respiratory syncytial virus (RSV) is a seasonal respiratory virus that resembles the common cold, but can develop into a more serious illness for some people.
Each year, this virus spikes during cold weather months, typically late fall. This cycle, the CDC surveillance noticed that the peak is happening earlier than usual across the country, and hospitals are seeing more patients coming in with RSV.
The symptoms of RSV appear within a week after exposure, and they can include a series of effects lasting one to two weeks, such as:
For infants under one year old, the symptoms can be difficult to identify and can include the following:
For most people, the RSV virus is not dangerous. The immune system naturally takes care of the virus with a one-to-two-week recovery period. Some populations are at a higher risk (babies under the age of one) of developing serious complications, including:
RSV is so common that most children contract and recover from RSV before turning two years old. Having RSV isn’t necessarily a cause for concern—but keep a close eye on the more troubling symptoms involving difficulty breathing and look for signs of dehydration.
Infants, the elderly, and those with compromised immune systems or existing breathing problems are at a higher risk when it comes to RSV. Their bodies may struggle more than others to heal from the virus and may require medical intervention.
Here’s a list of specific factors that may also put you or your loved ones at a higher risk of RSV-related complications:
If you or someone in your family is at a higher risk of complications from RSV, then follow the precautions in the next section to reduce your chances of exposure. If you have a trip planned to Vegas with your infant, you may want to reschedule until your baby is older and the spike in RSV has passed for the season.
Follow these tips to help reduce the spread of RSV in Las Vegas and elsewhere:
If you believe you or your child has RSV, stay home for at least one week after symptoms begin. Schools and daycares tend to spread RSV. People with cold or flu-like symptoms should avoid contact with those who are at a higher risk of complications from RSV until they have recovered.
RSV testing is available. There are several types of tests that can be used to diagnose the viral infection. Testing is recommended for more vulnerable populations with symptoms who are at a higher risk of developing severe respiratory infections from the virus.
The testing process varies but one method is very similar to Covid-19 testing; using a nasal swab. Another method requires flushing the nose with saline liquid to collect the sample for lab testing.
In most cases, RSV clears up on its own, and no medical intervention is required. There are not currently any vaccines or medications that are used for recovering from RSV.
Here are some natural remedies that help to relieve the symptoms:
If you need help treating the symptoms and over-the-counter medications are not helping, or you’re not sure about giving your child cold medicine, contact your doctor or pediatrician.
In rare cases, infants or older adults may require treatment in a hospital setting for a few days so that they can get oxygen or IV fluids to help with breathing and hydration while the body recovers. Out of 100 infants under six months old who test positive for RSV, only one or two will require hospitalization.
RSV is a common virus that comes around every year and doesn’t pose much of a problem for most people. However, for some, it can become life-threatening. If you or someone in your family is at a higher risk for RSV-related complications and you’re concerned, there are steps you can take to minimize your exposure.
If you’re having symptoms and would like to get tested for RSV because you or someone you are around frequently is at a high risk for complications, contact My Virtual Physician to set up RSV testing or get medical advice to treat symptoms.
Book Appointment Now Call For An Appointment

My Virtual Physician has an exciting announcement to celebrate: our hybrid clinic on Paradise Road is now open in Las Vegas!
My Virtual Physician’s mission is to provide safe, secure, and convenient access to healthcare for men, women, and children. In other words, we use telemedicine to fill the healthcare access gap that’s left by the reality that many doctors don’t offer same-day services. Patients who need to see a doctor now have the ability to meet virtually with our team of physicians with same-day appointments.
Our online telemedicine services launched during the pandemic, have grown exponentially, and continue strong today—providing quality healthcare access nationwide, online. We credit our growing team of doctors for our success.
But My Virtual Physician aims higher than simply providing online access to those who have the right equipment for a virtual visit (such as a smartphone or computer equipped with a camera and mic).
Other limitations exist with providing this type of healthcare solely online, including not having a private or safe place to interact virtually and the lack of medical equipment for taking vitals and collecting labs for diagnostics.
To overcome this challenge, My Virtual Physician opened its first one-of-a-kind hybrid clinic in Las Vegas. We’re excited to announce that, despite some major obstacles, we have successfully launched our first physical walk-in location.
Related: Hybrid Medical Clinics: Expanding OBGYN Access in Las Vegas
My Virtual Physician’s hybrid medical clinic is now open at 2217 Paradise Road in Las Vegas. Walk-ins are welcome. Find out our current hours or book an appointment (if preferred) here.
We are pleased to welcome men, women, and children into the physical clinic for a virtual visit in our private patient room, where our videoconferencing equipment is already set up and ready to go. We provide women’s health, pediatric, and primary care services in our hybrid clinic.
My Virtual Physician is proud to have opened the first clinic in Vegas that offers immediate access to online healthcare for those who may not have access to the equipment or private space. We welcome all to come visit us. Find us on Paradise Road! Get Directions Here.
Related: Now Available: Walk-in STD Testing in Las Vegas at Hybrid Clinic
 Inside Our Las Vegas Hybrid Clinic
Inside Our Las Vegas Hybrid ClinicTake a peek inside our clinic, where our certified medical assistant (CMA) will greet you! We have a comfortable waiting room for busier times. We also have a private room for patient use where our CMA will take your vitals, give you the tools to collect samples if needed for labs, and then you can meet virtually with our doctors with our private and secure videoconferencing setup.
At times, we do staff the clinic with a nurse manager and other medical professionals who can provide additional services such as wound care, vaccinations, ultrasounds, and more. If you’re interested in these services, please call ahead to (888) 224-0804 so that we can make sure the appropriate staff is present for your visit.
My Virtual Physician offers affordable and immediate access to patients at our new hybrid clinic in Las Vegas. Click to find out more about which services we offer. Welcome to our clinic!
Did you know that the CDC reports nearly 700 Americans die each summer from extreme heat? Higher outdoor temperatures can lead to hyperthermia (high body temperature), ultimately resulting in complications. It's August, and we are getting closer to fall. However, summer is not over yet.
Prolonged heat exposure in the summer months can cause heat stroke and dehydration. What's more, extreme heat can worsen certain health concerns, including heart problems. Complications and illnesses due to heat are preventable.
Here we explain why high summer temperatures are concerning and what precautions you should take this summer.

Intense heat presents a health risk for everyone, especially those with heart conditions. They face danger and even an increased risk of death. That is because the way that our bodies adjust to heat can cause internal stress and even restrict blood flow. Also, blood pressure can increase when the body tries to cool itself, which strains vessels and the heart.
If you have ever had a stroke or a heart attack, your body may not be strong enough to compensate for the strain caused by extreme heat. If you start to feel sick or extremely uncomfortable from the heat, it could be a sign that something is going on. So, you should take action to calm and cool the body.
Here are a few ways to help your body manage the stress of extreme temperatures this summer.
During the summer, you must stay hydrated. Taking in enough fluids each day is essential to avoiding heat-related complications. Unless your doctor restricts your fluid intake because of heart or kidney disease, you should drink plenty of water. Avoid caffeinated beverages. Also, eat fruits that are high in water content, such as:
Fruits also contain fiber, which can help balance your body's hydration.
Note: If your doctor has limited your water intake, ask how much you should drink this summer.
This summer, avoiding sugary drinks like soda and juices would be best because they may increase the risks of high blood pressure, obesity and diabetes. They can also lead to a "sugar crash," which can drain your energy and harm your teeth.
Salts and other minerals in the body are essential for vital body functions, including:
Heavy sweating during the summer results in loss of electrolytes, like salts and minerals. It is best to replenish electrolytes during this season through a balanced diet. Consider adding a multivitamin to your diet to stay healthy so that you will be able to avoid heat-related health complications this summer.
If you are going to be outside during the summer, experts recommend wearing loose-fitting, lightweight, and light-colored clothes. Light color clothes absorb less heat and may reflect the sun's rays compared to dark colors and heavy clothes.
In extreme heat, it is best to stay indoors in air-conditioned places. If you do not have air-conditioning at home, you could go to a public place like the library. Resting in air-conditioned buildings for part of the day will cool your body. Remember that fans can make you comfortable but may not prevent heat-related complications when the temperature is very high.
If you don't have adequate air conditioning, you can also try to take a cool bath or shower.
Avoid using your stove and oven as much as possible to keep your home cool.
If you must be outside, try to schedule outdoor activities during the coolest times of day, morning and evening hours. Rest in shady areas.
It is important to use sunblock because sunburn reduces your body's ability to cool down. It also makes you vulnerable to dehydration.
You may be able to prevent sunburn by wearing hats, sunglasses, and a broad-spectrum sunscreen outdoors. Try to apply SPF 15 or higher sunscreen 30 minutes before going outdoors.
Although anyone can suffer from heat-related complications, some people are at higher risk. These may include:
If you have loved ones at risk this summer, visit them or check on them frequently, especially during the day. Children and older adults may need extra help during summer.
Also, watch local news updates on extreme temperatures and safety precautions.
If you or someone you know is not tolerating extreme heat this summer, here are some of the signs and symptoms you might notice.
If you are with someone who complains of these heat-related symptoms, help them find a place to rest and cool off with a fan and a cold towel. Call a healthcare provider if the symptoms do not improve.
Talk with one of our expert doctors if you want to learn more about virtual services. My Virtual Physician offers video consultations for non-emergency care to older adults and children. If you need to see a doctor, book now.
Contact us today to find out how you can book a consultation appointment.
Disclaimer: The contents of this article are for informational purposes only and do not constitute medical advice. The information, graphics, and images on this site are not intended to substitute diagnosis or treatment by a medical professional. Always seek the advice of a licensed physician for any questions you may have regarding a specific condition.
“Extreme Weather and Your Heart: What You Need to Know When It Gets Really HOT!”. secondscount.org. Accessed July 31, 2022.
“Heat Exposure and Cardiovascular Health: A Summary for Health Departments”. cdc.gov. Accessed July 31, 2022.
“Heat-related health dangers for older adults soar during the summer”. nih.gov. Accessed July 31, 2022.
"Work Clothing and Personal Protective Equipment (PPE) Elements of Your Written Program and Effective Work Practices". dir.ca.gov. Accessed July 31, 2022.
“15 Water Rich Fruits To Keep Your Hydrated in Summer | List Of Water Rich Fruits | Fruits With Highest Water Content”. seniority.in. Accessed July 31, 2022.
Sarah Falcone, BSN, RN, WCN-C, CSWD-C, is a registered nurse in Fort Worth, TX. She works with clients in home health, wound care, and telemedicine. Sarah is a passionate advocate for moving advanced levels of care to the home, where her clients can safely receive the medical treatments they need with greater satisfaction and comfort. She focuses on patient experience, outcomes, and advancing clinical models using innovative technology to serve patients better. Sarah draws from 15 years of practicing patient care and nursing leadership to share her own nursing experiences and expertise online. Connect with her on LinkedIn!
Telemedicine provides a convenient way to get the care you need without traveling to the doctor or specialist you need. Virtual care, or Telehealth, has been around for a while, but recent changes in healthcare have caused telemedicine services to surge.
In the past, telemedicine visits were used primarily as urgent care encounters. If you had symptoms of a cold, you could chat with a Tel-a-doc and maybe get antibiotics.
Today, telemedicine services have expanded. And patients can see their telemedicine doctor for gynecologic, primary, and even wound care. In this post, we will look at how telemedicine has become a solution for patients with chronic or non-healing wounds by answering these questions.
Read on to learn more about telemedicine as a wound care solution.
Telemedicine is a healthcare delivery model that involves virtual consultations between patients and physicians, using online tools such as video conferencing, virtual examination rooms, and remote medical devices.
In many situations, telemedicine is ideal for individuals with wounds.
Those injured or struggling with chronic wounds may not feel like leaving home. Or they may be physically unable to leave home without assistance.
Often their caregivers work and cannot take time from work for frequent doctor appointments. Also, depending on where an individual lives, there may not be a wound specialist in the area. If there is a local certified wound care expert, they may have limited availability.
So, wound care appointments may be difficult to get.
Telemedicine providers with specialized training and certification in wound care can save patients and their families frequent trips to their doctor or wound clinic. Telemedicine for wound care is efficient. Doctors can conduct virtual visits, see the wounds, and make treatment recommendations through video.
Telemedicine also lets patients have virtual follow-up conversations with their doctors and send images when the wounds change.
Telemedicine decreases costs by reducing the need to travel long distances to the hospital or to consult with a physician. It improves the quality of life for patients with chronic wounds while maintaining high standards of wound care.
Since the COVID-19 pandemic, federal and state programs (Medicare and Medicaid) and private insurers have expanded coverage for telemedicine services, including wound care.
That is good news for patients with wounds who need to see a specialist. In many cases, your health insurance will cover the cost of your virtual visit and wound care supplies that your provider orders.
Your insurance may cover a virtual doctor visit for treatment if you have:
You can check with your insurance company to find out what they will cover or talk with a telemedicine provider and have them verify your insurance coverage before making an appointment.
Wound care specialists provide a variety of services through telemedicine. According to the Department of Health and Human Services, Telehealth services are especially helpful for monitoring and improving ongoing health issues, like chronic wounds.
A telemedicine wound care specialist can evaluate and treat wounds virtually by:
These services help patients get the right treatment to heal the wound quickly and return to normal lives.
Telemedicine specialists also coordinate your care with your other doctors or home health.
There are many advantages of using telemedicine wound care services, including:
It’s easy to see why telemedicine wound care services are growing.
While there are numerous benefits of telemedicine for patients, primary among them is the ease of convenience and the ability to access quality care fast. Wound care services provided through telemedicine are a great example of a wound care solution that is helping many individuals get the care they need.
If you have a skin wound that needs medical attention, talk with the My Virtual Physician team to find out if their telemedicine wound care services are right for you.
Contact us now for your low-cost appointment that your insurance may cover!
Telemedicine, also known as telehealth, improves access to healthcare without being physically present at a healthcare facility. Over digital devices with an internet connection, people can speak with a doctor and get all the help they need.
Although introduced in the late 1950s, the need and use of telehealth services recently peaked during the Covid-19 pandemic. For several reasons including lockdown restrictions, fear of getting infected, and increased burden on the healthcare system, thousands of people could not leave their homes to visit a healthcare facility. While things are seemingly back to normal, telemedicine might be here to stay for good.
The question then arises, does my health insurance cover telehealth? The answer is music to the ears. Medicare covers a wide range of medical and health-related services, and that includes telehealth. In this article, we will discuss what parts of Medicare cover telehealth services.
Book Appointment Now Call For An Appointment
Medicare is made up of different parts namely:
Each of these parts covers different medical and health-related services. Telehealth is covered by Medicare parts B and C.
Medicare Part B covers outpatient services, and since telehealth visits are treated as such, it covers telehealth services. Hence, you may enjoy the services of the following health professionals:
According to the Centers for Medicare & Medicaid Services (CMS), the outpatient-related telehealth services you may enjoy include:
Additionally, the price is the same. The amount people with Medicare pay for in-person outpatient services is the same amount for telehealth services. According to the CMS, Medicare covers 80% while the personal pays 20% of the cost of standard services. Some of these healthcare services may start with an in-person visit and continue with virtual visits.
Medicare Part B can also cover emergency (ambulance) transportation and limited non-emergency rides. So, if a client with Medicare needs transportation to a healthcare facility for follow-up care, its cost may be covered. The same goes for non-emergency transportation. If a client is nonambulatory or needs monitoring in transit to another facility, the cost of transportation may be covered. Clients are to check if Medicare can cover their transportation needs.
Medicare Part C, also known as Medicare Advantage is sold by private insurance companies. In 2020, it was upgraded to provide increased access to telemedicine services from home. Generally, it has the same coverage for telehealth services as original Medicare (Part A and B) but may come with additional benefits.
Since it is provided by private insurance companies, the plans may be different. Individuals should check their specific plans with their insurance provider to know what telehealth services they are entitled to enjoy.
At My Virtual Physician, we are in-network with many insurance health plans including Medicaid, Medicare, United HealthCare, and Blue Cross.
Our team is committed to ensuring that patients get the best of health care as needed. We provide virtual care at any point in your pregnancy while you await your appointment with your local OB doctor. We are also available to help guide you through your pregnancy and answer any questions that may arise.
Book Appointment Now Call For An Appointment
Every 13 minutes, a woman dies from breast cancer. Unfortunately, many women with the disease do not show symptoms. So, regular screening for breast cancer is critical for early detection and diagnosis.
Breast Cancer screening typically occurs as a part of routine preventative care. Individuals do not have to have any signs or symptoms to have a screening performed by their doctor. Manual exams, ultrasound, thermography, and mammography are a few ways patients are screened for abnormalities. A doctor can explain screening options and when it is time to consider certain tests.
To find out how breast cancer screening aids in the diagnosis of the disease, read on.

Breast cancer can be asymptomatic. In other words, it may have no symptoms. In fact, cases may show different symptoms and examination findings. That is why screening should be individualized for each patient.
Screening means looking for or testing for something when there are no signs.
Many people think that only someone with a family history should worry. Yet, about 85% of breast cancers occur in women who do not have any family history of breast cancer. Rather, genetic mutations that occur as women age increase their risk. The most significant risk factors for breast cancer are being a woman and growing older.
Doctors are trained in the latest research and guidelines. They can tell their patients about the options. And doctors help women decide when it is a good idea to be tested.
Breast cancer is typically diagnosed in one of the following ways:
Mammography is the most common screening method used today. Other testing methods include Digital Breast Tomosynthesis (DBI) and thermography, although these are not widely used.
According to a recent article, doctors are seeing later-stage cancer cases in younger women. This is worrisome because cancers detected in younger women in their 20s and 30s are more aggressive. And they may lead to poorer outcomes.
Doctors are seeing later-stage cancer cases in younger women. This is worrisome.
Early detection is key in cancer treatment. The cost of treatment, risks of complications including death, and length of treatment go down with earlier detection.
If not caught early, cancers can grow and spread. When cancer cells move to other organs, this is called metastasis. Thus, cancer is harder to treat.
The best way to catch cancerous changes early is through regular check-ups with a doctor and routine screening tests to help detect changes early. Online doctors or virtual gynecologists can order mammograms or other imaging tests, and tailor screening plans for women who do not usually see a primary care physician.
Medical researchers continue to look for ways to help doctors with better and more accurate tests.
In 2019, the National Cancer Institute presented a new study that showed Doctors could detect breast cancer up to five years before any clinical signs appear, using a blood test for tumor-associated antigens (TAAs).
Newer research from Johns Hopkins University School of Medicine paired blood tests with other screening tests to determine whether finding and treating cancers identified by blood tests reduced mortality rates. Researchers said that “some screening may actually cause more harm than good.” And so, they used bloodwork with standard imaging procedures.
Results were promising. Researchers concluded that there is hope for a blood test that could eventually reduce deaths from cancers that typically go undetected until late stages. But “any blood test needs to complement and add to standard-of-care screening because standard-of-care screening works.”
Current recommendations encourage most women to have a mammogram beginning at age 40. Here are the most recent guidelines on screening.
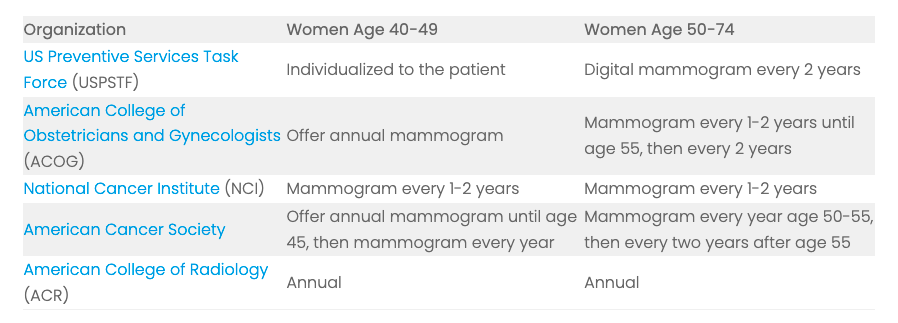
My Virtual Physician can offers virtual gynecology services in many states. Women can talk with experts about individualized screening plans. Don’t worry about your risk. Talk to the doctor now.
My Virtual Physician is now accepting new patients.