Many Americans faced job losses this year. That means that a lot of families lost their health insurance. That leaves many wondering, can you make a doctor's appointment without insurance?
Doctors and healthcare facilities allow individuals to book appointments without insurance. When scheduling an appointment, patients are asked about who will pay for the services. Without health insurance, it is possible to pay out-of-pocket. If paying for treatment without insurance coverage, it is important to consider factors like necessity and cost.
Here's what you need to know when booking a doctor's appointment without insurance.

Healthcare providers, like doctors, treat patients' health concerns. When it is time to see a physician, the first step is to contact them for an appointment.
To make an appointment to see the doctor, patients will need these things:
Those who are not covered by a health insurance plan can still schedule an appointment. The doctor's office will charge the patient directly instead of billing an insurance company.
Making a doctor's appointment without insurance is just like making an appointment with coverage. In most situations, patients can receive the same treatment.
Sometimes a test or medication is very expensive without insurance. However, doctors will often discuss what treatments or procedures are necessary and how costly they may be. That is why it is good to talk with a doctor even if you don't have insurance.
A recent poll found that about 44% of Americans would not go to the doctor if sick or injured because of the cost.
Many providers offer discounts for cash-paying customers. Others may be able to arrange payment plans. There is nothing more valuable than your health. Skipping the doctor because you don't have insurance is a bad idea.
An average doctor's appointment costs between $68 and $234, according to Debt.org. The charge may change depending on how difficult the condition is and how much time the doctor spends with the patient.
One cost-saving alternative to an in-office appointment is telemedicine. Online doctors offer significant savings to patients, including the expense of time and travel. And some online doctors offer reduced visit fees as well.
Even those with insurance can benefit from saving money on gas and cutting the wait time by booking a virtual physician appointment. All of the top private health insurers offer some telehealth coverage.
My Virtual Physician offers the best in telemedicine services. They regularly add new insurance plans, but those without insurance can see a doctor today for only $49.99. Each patient at My Virtual Physician receives patient-focused, quality care with or without health coverage.
If you've experienced a job change or lost health insurance coverage, check with My Virtual Physician for a doctor near you. Book now with the secure patient portal. And get the care you need.
Did you know that My Virtual Physician is now accepting SilverSummit Health Insurance? That is great news for residents of Nevada’s Clark and Washoe counties. Members can now book an online doctor appointment with no out-of-pocket expense.
SilverSummit Healthplan provides the best Nevada Medicaid plans. Now they are adding even more value to their services by partnering with My Virtual Physician to give members virtual doctor visits. Residents of Nevada can access doctors to treat a wide range of problems, including:
My Virtual Physician’s caring doctors treat patients right in their own home through a video visit. The office provides appointments for Obstetrics/Gynecology (OB/GYN) or Primary Care Physician (PCP) services. And patients can book safely and easily through the patient portal.
Health insurance plans are similar because they usually cover the same services. But different plans may:
Some plans are Health Maintenance Organizations (HMOs). These give members a list of doctors to choose from in their network. Insurance will cover services from in-network doctors, but may not cover the same services with out-of-network providers. My Virtual Physician is thrilled to add SilverSummit to their accepted Insurance Plans lineup and accept new patients.
My Virtual Physician is still adding new insurance plans to the network. But even without insurance, visits are still less expensive than an in-office visit. And the office accepts many forms of payment. Patients also appreciate booking an online doctor appointment because it is more convenient. My Virtual Physician has late evening and weekend appointments for booking. Members of SilverSummit Healthplan can schedule an appointment now at www.myvirtualphysician.com or text the office staff with questions.
To meet the physicians, simply click “BOOK APPOINTMENT NOW” to book your visit. Or visitors can text message questions about the virtual/online doctor benefits.
Every 13 minutes, a woman dies from breast cancer. Unfortunately, many women with the disease do not show symptoms. So, regular screening for breast cancer is critical for early detection and diagnosis.
Breast Cancer screening typically occurs as a part of routine preventative care. Individuals do not have to have any signs or symptoms to have a screening performed by their doctor. Manual exams, ultrasound, thermography, and mammography are a few ways patients are screened for abnormalities. A doctor can explain screening options and when it is time to consider certain tests.
To find out how breast cancer screening aids in the diagnosis of the disease, read on.

Breast cancer can be asymptomatic. In other words, it may have no symptoms. In fact, cases may show different symptoms and examination findings. That is why screening should be individualized for each patient.
Screening means looking for or testing for something when there are no signs.
Many people think that only someone with a family history should worry. Yet, about 85% of breast cancers occur in women who do not have any family history of breast cancer. Rather, genetic mutations that occur as women age increase their risk. The most significant risk factors for breast cancer are being a woman and growing older.
Doctors are trained in the latest research and guidelines. They can tell their patients about the options. And doctors help women decide when it is a good idea to be tested.
Breast cancer is typically diagnosed in one of the following ways:
Mammography is the most common screening method used today. Other testing methods include Digital Breast Tomosynthesis (DBI) and thermography, although these are not widely used.
According to a recent article, doctors are seeing later-stage cancer cases in younger women. This is worrisome because cancers detected in younger women in their 20s and 30s are more aggressive. And they may lead to poorer outcomes.
Doctors are seeing later-stage cancer cases in younger women. This is worrisome.
Early detection is key in cancer treatment. The cost of treatment, risks of complications including death, and length of treatment go down with earlier detection.
If not caught early, cancers can grow and spread. When cancer cells move to other organs, this is called metastasis. Thus, cancer is harder to treat.
The best way to catch cancerous changes early is through regular check-ups with a doctor and routine screening tests to help detect changes early. Online doctors or virtual gynecologists can order mammograms or other imaging tests, and tailor screening plans for women who do not usually see a primary care physician.
Medical researchers continue to look for ways to help doctors with better and more accurate tests.
In 2019, the National Cancer Institute presented a new study that showed Doctors could detect breast cancer up to five years before any clinical signs appear, using a blood test for tumor-associated antigens (TAAs).
Newer research from Johns Hopkins University School of Medicine paired blood tests with other screening tests to determine whether finding and treating cancers identified by blood tests reduced mortality rates. Researchers said that “some screening may actually cause more harm than good.” And so, they used bloodwork with standard imaging procedures.
Results were promising. Researchers concluded that there is hope for a blood test that could eventually reduce deaths from cancers that typically go undetected until late stages. But “any blood test needs to complement and add to standard-of-care screening because standard-of-care screening works.”
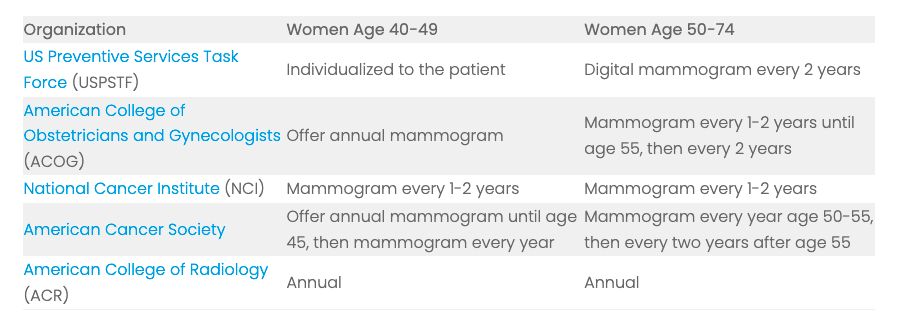
Current recommendations encourage most women to have a mammogram beginning at age 40. Here are the most recent guidelines on screening.
My Virtual Physician can offers virtual gynecology services in many states. Women can talk with experts about individualized screening plans. Don’t worry about your risk. Talk to the doctor now.
My Virtual Physician is now accepting new patients.
My Virtual Physician has great news to share. Nevada’s favorite telemedicine provider is now in-network with Anthem Blue Cross Blue Shield (BCBS). Nevada residents looking for an online doctor may be able to book an appointment now with little to no out-of-pocket expense.
Anthem leads the health insurance industry with a strong desire to make healthcare easier and change lives. Anthem health plans serve more than 42 million families. That is why My Virtual Physician (MVP) is proud to join the Anthem Nevada provider network.
BCBS is known for offering members value-added services.

Anthem Nevada’s member support services are unmatched.
And when Anthem Nevada members need to see a doctor, that’s where MVP comes in. Their board-certified, expert doctors care for Nevada patients from the convenience and safety of home.
MVP offers Obstetrics/Gynecology (OB/GYN) and primary care services to residents of Nevada. Whether using insurance or paying out-of-pocket, My Virtual Physician’s pricing is competitive, and the patient care is unmatched.
Take a look at a few of the current online physician services they treat for Nevada residents:
Patients who need to see an online doctor can book now through a secure patient portal. My Virtual Physician is excited about the new Anthem Nevada partnership and is now accepting new patients. Virtual doctor visits are now easier than ever.
Residents of Nevada can find more information about Anthem BCBS in Nevada at www.anthem.com.
To meet our book an online doctor appointment with our physicians, simply click “Book Appointment Now” to book your visit. Or visitors can contact the office for questions about their virtual/online doctor benefits. My Virtual Physician is standing by to help.
Have you been looking for a Nevada healthcare provider that is in your Prominence Health Plan network? Look no further.
My Virtual Physician (MVP) is excited to announce a new partnership with Prominence Health Plan. Prominence is a respected plan provider that offers a broad network of hospital and healthcare services to its members. Together, MVP and Prominence are serving more individuals with the high quality online healthcare services they need.
Here’s what this new relationship can do for you.

Prominence Health Plan is a subsidiary of Universal Health Services (UHS), which was recognized by Fortune and Forbes as a top company in 2021.
Prominence focuses on providing their members with options for quality, convenient, cost-effective care close to home.
Prominence Health Plan began in Reno, Nevada as a commercial Health Maintenance Organization (HMO) in 1993. Since then, they have expanded to include Preferred Provider Organization (PPO) and Medicare Advantage (MA) service lines in multiple states including Nevada, Texas, and Florida.
What Does Prominence Cover?
Prominence Health Plan, like most insurers, offers different types of medical plans. Health insurance plans are similar because they cover many of the same services. Yet they can be different when it comes to:
If a plan is called a Health Maintenance Organization (HMO), the insurance plan gives members a list of doctors that are in the network. Choosing a provider that is not on the list may mean that the insurance will not cover any of the visit costs. Members are encouraged to choose an in-network provider so the services will be covered by the plan.
On the other hand, if a plan is called a Preferred Provider Organization (PPO) the member has more options. They can pick any doctor. But choosing an in-network doctor makes services more affordable because of discounts or additional coverage for using in-network providers.
It is easy to see why it is best if your doctor is in-network with your insurance plan. This is one reason why MVP is excited to announce that they have joined the Prominence Health Plan network.
MVP and Prominence have a lot in common.
They both started in Nevada.
They are both well-respected companies.
And both work to provide options for quality, convenient, cost-effective care close to home.
Prominence Health Plan and MVP are a perfect match.
MVP is a multi-specialty telemedicine team, treating patients across the US. They provide comprehensive online doctor visits to treat patients of all ages with care for obstetrical-gynecological, primary care, and pediatric services.
Virtual physician appointments are affordable and easy-to-schedule. Plus, they offer the safety and security of being seen from your home or workplace in convenient after-hours and weekend appointment times. Now with more in-network insurance coverage, MVP’s online physician services are better than ever.
MVP’s online doctors treat gynecological issues including:
As well as primary care concerns such as:
If you need to see a doctor and you’ve been looking for the best care at an affordable price, your search can stop here.
Many health concerns can be solved with a simple online consultation. The team at MVP is available now to meet with you.
Did you know My Virtual Physician is offering a promotion for September? Book now to get a free home blood pressure kit for new patients who complete an online consultation in the month of September. Don’t wait, grab your appointment spot now!
MVP’s founder Dr. Howard is a board-certified physician practicing in Las Vegas, Nevada. He is passionate about medicine and research. He has authored/co-authored several publications and is among the top 10% of scientific reviewers in the United States. Dr. Howard and his team are now accepting new patients.
Women looking for a great Obstetrics and Gynecology provider (OB/GYN) in Las Vegas, Nevada, may have trouble. There is an OB/GYN physician shortage in Las Vegas. And the situation is getting worse.
Factors such as physician burnout, population growth, and competition from other parts of the country have created a shortage of OB/GYNs in Las Vegas, Nevada. As a result, some may have difficulty finding the perfect provider to care for their reproductive health.
Women and their partners want an OB/GYN they can trust. Issues like birth control, childbirth, and menopause are delicate matters. Unfortunately, a shortage means there are not enough providers to meet Las Vegas’ needs. Thus, those doctors who are available may be overworked or stretched thin.
Here is why it’s hard to find a good OB/GYN in Las Vegas and what to do about it.

When there are too few doctors to meet a city's demands, it can be hard to find a provider to respond to each patient’s needs. According to NBC News, America is facing an OB/GYN shortage.
Las Vegas, overall, has the most severe OB/GYN workforce shortage.
Other parts of Nevada face an even more serious situation. Some counties lack even one OB/GYN provider. Hence, patients face delays in care. In some cases they are forced to look far away to find a doctor.
Here’s why it is hard to find OB/GYN care in Las Vegas.
And while Las Vegas OB/GYNs may have it rough, the patients suffer too.
OB/GYNs offer services that women need. They provide health counseling, sexually transmitted infection (STI) testing, and more. From puberty to menopause, women need a health expert they can trust. Many patients depend on OB/GYN advice.
Fortunately, Las Vegas residents can now find the best OB/GYNs, right in their neighborhood.
My Virtual Physician has an answer for the physician shortage crisis. Two of the best board-certified OB/GYNs in the nation are on staff and available for appointments near you in Las Vegas.
My Virtual Physician offers OB/GYN visits in Las Vegas with flexible scheduling through telemedicine. While most providers are busy and feel the pressure to treat many patients quickly, My Virtual Physician is different. Online video visits eliminate travel time and the feel of a busy waiting room. Virtual consultations provide a relaxed, personalized, and patient-centered care experience.
During the pandemic, many patients have had questions about staying safe. Some want to know if vaccination is right for them. Women in Las Vegas can now book a visit with My Virtual Physician to discuss their concerns and get real medical advice. Booking an appointment with an OB/GYN in Las Vegas has never been easier.
Are you looking for an OBGYN near you in Las Vegas? My Virtual Physician has two board-certified physicians licensed in Nevada who can address gynecological problems via video visits.
If you would like to talk with a board-certified OB/GYN, you can schedule your appointment online now. My Virtual Physician offers health screening, lab tests, and counseling to meet all of your healthcare needs.
This past year tested many young businesses. Telemedicine is not new. But the My Virtual Physician (MVP) business model is. The virtual doctor practice offers the best in online doctor services as a direct-to-consumer multi-specialty provider licensed in multiple states. Regardless of 2020's challenges, the MVP virtual doctor team didn't slow down. They focused on their path to becoming the #1 online doctor and forged ahead.
Over the last 12 months, MVP worked hard to bring high-quality medical care into homes in 15 states. They now offer online pediatric, gynecologic, and primary healthcare services for patients of all ages. Plus, they provide same-day scheduling for online physician appointments, some in-network insurance benefits, and five-star customer service.
As the #1 online healthcare provider, MVP doctors get to know their patients. Quality care is emphasized, and they aim to provide the best patient satisfaction in telemedicine. Here’s what patients are saying about MVP's online doctors:
“I would give My Virtual Physician more stars if I could”
“Dr. Howard has the best personality and is very friendly.”
“The future of medical visits; what better way to social distance.”
“A+ would recommend to everyone.”
Since their launch, MVP has opened new offices and added service lines such as nutrition and diabetic care. The practice has partnered with more online doctors and added office staff. Just this Spring, MVP enhanced their patient portal for self-scheduling, and integrated a program to trend patient reviews.
This one year anniversary milestone is cause for celebration. It is exciting, and this is only the beginning. Despite any challenges that lie ahead for this medical practice, their progress shows that the future is very bright for My Virtual Physician.
Congratulations to Dr. Howard, Dr. Masghati, Dr. Ayyagari, and all of the My Virtual Physician Staff.


My Virtual Physician now offers virtual doctor visits in Las Vegas. Their telemedicine visits offer comprehensive services in the following areas:
In the middle of a pandemic, along with a cold and flu season, many residents fear going out in public. Due to high patient volume, Las Vegas physician offices are busy. In some cases, patients can't get an appointment with their physician when they need it... until now. Las Vegas residents can now conveniently access a virtual doctor with My Virtual Physician.
Patients emphasize the convenience of having an online doctor visit where they receive the personalize care they need, all from the comfort, privacy, and safety of their homes. Patients can skip the waiting rooms and old magazines and enjoy waiting for their appointment in their own home. When it comes time to talking with the provider, their doctor is ready to connect and focus with them one on one. My Virtual Physician can effectively treat the following gynecology conditions during an online visit:
Our patients rave about our primary care services. The virtual doctors at My Virtual Physician understand getting to know their patients, their medical histories, and the factors impacting health and wellness. With top-notch and on-demand Las Vegas primary care telemedicine services, My Virtual Physician can effectively treat patient health concerns involving:
Residents in Las Vegas, Nevada can schedule a virtual doctor appointment or choose a provider through a secure and fast online booking system. Our Las Vegas OBGYN accepts Medicaid. Contact us to learn more about our services!
Starting a family is a goal for many couples. Unfortunately, one in ten couples may have some difficulty getting pregnant and require medical treatment. If you've been affected, you might be wondering about infertility: when is it time to see a doctor? My Virtual Physician has board certified physicians who specialize in infertility and are available for virtual doctor visits.
Infertility is a diagnosable medical condition in which a couple cannot conceive a pregnancy despite unprotected intercourse. It can be caused by many factors.
In women, most often, abnormal ovulation causes infertility. In men, usually problems with sperm cells, such as sperm count or function, cause difficulty conceiving.
Aside from these physiological causes, factors affecting a couple's fertility include their age, health status, and lifestyle factors such as stress, diet, or smoking.
According to the American College of Obstetricians and Gynecologists, women who are overweight, underweight, or exercise too much may have difficulty getting pregnant, and men who are heavy drinkers or smoke marijuana since these are known to lower sperm count and movement.
In some cases, doctors cannot determine the cause and refer to these cases as unexplained infertility.
Generally, it is time to consult your physician about getting pregnant if you are under the age of 35 and have been unable to conceive after one year of unprotected sex. Women over the age of 35 and those who have irregular menstrual cycles or have known abnormalities with their reproductive system, should talk with their doctor much sooner, after six months.
Infertility affects both people in the relationship. There is a 30% chance the infertility is related to male factors in a traditional couple, 30% related to female factors, and a 30% chance a combination of both factors. Therefore, anyone in the relationship may need to discuss options for starting a family. Here are some reasons to see a virtual doctor:
When you consult your physician about infertility, you can expect that they will begin your care with a complete history and physical exam. They may order blood testing, urinalysis, hormone tests, or other diagnostics to check for abnormalities. It may be necessary to have your partner undergo an exam and diagnostic testing also. Your physician may order an ultrasound or an X-ray as well.
After all of the tests, you will meet with your physician to discuss the results and go over treatment options and recommendations. After you decide on the treatment plan that is best for you, you will receive support and guidance in your process to get pregnant.
Medical treatment and new technologies can increase your chances of getting pregnant. One or both partners in a couple may undergo treatment.
Medications may be taken by mouth or injected. There are drug therapies for both men and women aimed at increasing egg production or sperm count. A list of medicines frequently prescribed for infertility treatment can be found here.
In some cases, blockages, scar tissue, or abnormal growths require surgical intervention. Procedures may be laparoscopic: meaning performed through small incisions in the abdomen for a minimally-invasive procedure.
Today, the two most common infertility treatments are intrauterine insemination (IUI) and in vitro fertilization (IVF).
IUI is a procedure during which a physician injects sperm into the uterus at the ovulation time. This method is least invasive and most cost-effective but has lower success rates. The estimated success rate is 10-20% for a single cycle of IUI, but additional rounds increase chances, and in three to six cycles, the success rate is up to 80%.
IVF is a complicated procedure requiring surgical retrieval of a woman's eggs, fertilization in a laboratory, and then transferring the fertilized eggs back into the uterus. Women under the age of 35 can expect a 50% success rate for IVF treatment, but this process requires intense testing and monitoring and can cost $20,000 to $50,000.
Starting a family can be challenging, and your physician may offer options to guide you through the process. Infertility is a medical condition that affects many couples, and there are treatments available.
Need to talk to a physician now? My Virtual Physician has Board-Certified OB/GYN's that are available for virtual doctor appointments and are able to answer any questions you have and guide you in the right direction. The online doctors at My Virtual Physician, not only address infertility and reproductive endocrinology, but also irregular periods and painful periods, and many more gynecological conditions.
If you still have questions or you would like to discuss your problem with our board-certified OB/GYN specialists, click below to schedule an appointment. My Virtual Physician treats conditions, including infertility, irregular periods, sexually transmitted infections, and more. If you have any suggestions for additional topics you want to read about, let us know! Don’t forget to check out our podcasts for more and follow us on social media.
With much focus on the coronavirus this year, don't forget about another viral infection that threatens your health. Each year the Influenza virus affects 5-20% of Americans. This illness puts millions at risk of lost work and sick days, medical expenses, and possible health problems. A flu shot lowers that risk. You may be wondering, should you get a flu shot?
The Center for Disease Control and Prevention (CDC) recommends that everyone over the age of six months should be vaccinated against the flu virus this year. With a few exceptions, Americans need their shots around October or in early fall.
Many people worry about just how the flu shot will affect them. If you're one of these, keep on reading to find out what you should know about getting vaccinated this year.
The American Academy of Family Physicians (AAFP) recommends a yearly flu shot for everyone over six months old. This is because the flu vaccine can safely and effectively prevent severe illness.
Flu vaccines contain dead or weakened forms of the Influenza virus. Your cells begin to build up a natural defense system when they receive these parts of the virus. Then, your body creates antibodies. These proteins help your body fight infection. Antibodies work to keep you healthy later on if you are exposed to the flu virus.
The Journal of the American Medical Association (JAMA) recently looked at the best time to get your flu shot. In their study, researchers found that the U.S. flu season usually starts in December. After a flu shot, your body takes about two weeks to build up a response to the vaccine. Therefore, flu shots give the most protection when given in the fall, around October.
Vaccination is safe. Doctors have recommended flu vaccines for over 50 years. Over this time, a lot of research has evaluated the effectiveness and safety of immunizations. Certainly, the risk of serious reactions is low. Furthermore, manufacturers demonstrate the safety of their drugs before the FDA gives their approval.
The Advisory Committee on Immunization Practices (ACIP) warns some individuals to talk to their doctor about the flu shot if they have certain contraindications. This means a specific situation, condition, or factor that could make a treatment unsafe or even harmful.
For instance, egg allergy prevents some from getting a flu shot. This is a contraindication because manufacturers use eggs to make the vaccine. Therefore, the flu shot may contain trace amounts of ovalbumin (egg protein).
In addition to contraindications, there are precautions for some individuals. For example, those with a history of Guillain-Barre Syndrome or who have an illness with fever may want to discuss vaccination with their doctor.
The flu shot may cause reactions. These are typically mild and go away within 48 – 72 hours. They may include:
In some cases, more severe reactions occur. These could be signs of a rare allergic reaction to the vaccine. If these signs or symptoms arise, you must seek medical attention right away:
The risk of not getting vaccinated is getting sick. You could miss work or school, incur medical costs, or suffer mild to moderate health complications.
Most healthy adults deal with a minor case of the flu virus by staying home and taking over the counter medication to ease symptoms. The infection generally lasts 7-14 days.
On the other hand, those considered "high-risk" could suffer much more serious cases. Some possible complications include hospitalization and even death. Here are some factors that put you in the high-risk category:
In conclusion, you and your healthcare provider will decide if a flu shot is right for you. You must talk with your physician about your past history and risk factors to decide whether or not to be vaccinated.
Talk to your physician if you still have questions about the influenza vaccine. They can help you with additional information.
If you still have questions or you would like to discuss your medical condition with a specialist, click below to schedule an appointment. MyVirtualPhysician treats conditions like the common cold, flu-like illness, and more. If you have any suggestions for additional topics you want to read about, please let us know! Don't forget to follow us on social media.
Rubin R. Is It Possible to Get a Flu Shot Too Early? JAMA. 2018;320(22):2299–2301. DOI:10.1001/jama.2018.18373
In the United States, FDA-approved generic medications account for 90% of prescriptions filled. Your doctor or pharmacy may have asked you about your preference for a generic or brand name drug. This could have left you wondering: are generic medications the same as brand names?
Generic medications are not exactly the same as brand names. This is because generic medications can have different ingredients, look dissimilar, or have individual effects. In many ways, the FDA ensures that the medications are the same. But here is what you need to know about generic vs. brand name:
A lot of money goes into research, testing, and marketing before a company can introduce a new drug to the public. Then, they can patent their new medication and own the right to make and sell their product exclusively for five years. This short time allows manufacturers to recoup some of the costs associated with getting their new brand name drug to market.
The patent expires after that time. This means other companies can come along and produce the same medication under a different name. This “copy-cat” is considered a generic medication.
So you may be asking… what is the difference anyway? Well, in many ways a generic medication is like the brand name version. To be approved as a generic drug, the pharmacologic characteristics must be the same as the brand name. This means that generic medicines are the same when it comes to:
By contrast, generic medications can be approved with different inactive ingredients. So colors, additives, and fillers used to help with binding, flavoring, coloring, or preserving may not be the same. That means that your generic medication will likely look different. Trademark laws in the U.S. prevent drug makers from creating a version that looks exactly like the brand name.
The Federal Drug Administration (FDA) regulates generic drugs that are approved for sale in the United States. It provides a process that ensures the medications are safe, effective, and of sufficient quality. Keep in mind that the FDA also investigates complaints about all medications including side effects. They can issue a recall any time there is a concern for safety.
There are always risks and benefits associated with any medication. Everybody is different, and some are more sensitive to differences in the drugs.
Because the inactive ingredients are not the same, some individuals may notice differences when taking a generic medication vs. a brand name, but this is not always the case.
There have been reports of medications affecting patients differently.
For example, when the onset of effects is felt, how long the medication effects last, and even the side effects can vary when comparing drugs made by different companies or labs.
Keep in mind that some pharmaceutical companies produce both brand and generic forms of medication, so even some of the generics are very close to the original.
It is important to talk to your physician if you are concerned about a generic medication affecting you differently.
The FDA requires drug companies to prove generics are effective for treatment in the same way brand name medications are. Some generic medications have been on the market for years and shown to be as effective and a solid choice for some consumers.
Some individuals choose generic versions because they work just as well but cost much less than the brand name. Again, the company making the generic did not have to pass along the cost associated with getting a new drug to market.
So when a patient is going to be on a drug long-term or even for a lifetime, choosing a generic medication can save thousands of dollars a year in medical expenses. Lower costs may mean better compliance for some patients.
The savings to the individual are important, but it doesn’t stop there. When multiple manufacturers are able to make and sell a medication the competition can drive the cost down and makes healthcare more affordable for the public. Generic medicines save our healthcare system millions of dollars every year.
This answer may be different for each person. As with many choices in your health and medical care, you have to weigh the risks and benefits.
Is it worth it for you to spend more on a brand name medication? Cost is an important factor when deciding what is best. For example, when a person is on medication for a lifetime, opting for a generic version may save thousands of dollars in healthcare costs. On the contrary, generic medication for an acute illness that will resolve quickly could mean a different decision.
Today, many pharmacies routinely fill the generic versions for cost savings to the insurance companies and the customers. The FDA says that increasing the availability of generic drugs in the marketplace encourages competition in the pharmaceutical market which improves access to healthcare.
Although generic medications are not identical to their brand name counterparts, the FDA ensures that customers are getting safe, effective, quality options when they chose an approved generic. Although they may have different ingredients, appearances, and effects, the pharmacologic effects are the same. As with all medications, there are risks and benefits that should be weighed when making a personal choice.
If you would like to know more or have questions about your medications, our doctors are available for a virtual consultation. MyVirtualPhysician is a multi-specialty provider with physicians available for a consultation now. Click below to schedule an appointment. If you have any suggestions for additional topics you want to read about please let us know! Don’t forget to follow us on social media.
 The Centers for Medicare and Medicaid Services (CMS) have issued the advance copy of its proposed 2021 Physician Fee Schedule rule on August 3 of this year. It contains the new telehealth services which will be covered under Medicare, which has changed immensely since the previous year. Unlike last year, where CMS made only minor additions to telehealth services, the proposed changes for 2021 are substantial. The addition of enhanced telemedicine services is designed to more deliberately expand the use of telehealth technologies among Medicare beneficiaries, making healthcare more accessible to Americans.
The Centers for Medicare and Medicaid Services (CMS) have issued the advance copy of its proposed 2021 Physician Fee Schedule rule on August 3 of this year. It contains the new telehealth services which will be covered under Medicare, which has changed immensely since the previous year. Unlike last year, where CMS made only minor additions to telehealth services, the proposed changes for 2021 are substantial. The addition of enhanced telemedicine services is designed to more deliberately expand the use of telehealth technologies among Medicare beneficiaries, making healthcare more accessible to Americans.
The most notable change is to allow physicians to fulfill direct supervision requirements while remote, provided the physician is immediately available to engage via audio-video technology if needed. This change can greatly increase physician leverage and virtual oversight, including more incident-to billing options. Another notable change is CMS’ proposal to remove frequency limitations for facility inpatient-type telehealth services. Essentially, these proposed changes are intended to expand the type of services for which doctors can perform and be reimbursed for through telemedicine.
Medicare is making a big push to expand access to telemedicine among medicare beneficiaries. Below is an article written by Foley and Lardner LLP which discusses the new changes and proposed telehealth codes and explains how to submit public comments on the proposed rule.
CMS proposed changing the definition of direct supervision to allow the supervising physician to be remote and use real-time, interactive audio-video technology. This is a big change because the current definition of direct supervision requires the physician to be physically present in the office suite and immediately available to furnish assistance and direction throughout the performance of the procedure. (It does not require the physician to be physically present in the actual room when the service or procedure is performed.) If finalized, the change would be in effect through December 31, 2021 or the end of the Public Health Emergency (PHE), whichever is later.
Under this new definition, direct supervision requirements could be met if the supervising physician was immediately available to engage via audio-video technology. It does not require the physician’s real-time presence or observation of the service via interactive audio-video technology throughout the performance of the procedure. Audio-only technology is not sufficient to fulfill direct supervision requirements.
The new definition opens opportunities for telehealth and incident-to billing. CMS acknowledged there are no Medicare regulations that explicitly prohibit eligible distant site practitioners from billing for telehealth services provided incident-to their services. But because the current definition of direct supervision requires on-site presence of the billing clinician when the service is provided, it is difficult for a billing clinician to fulfill direct supervision of services provided via telehealth incident-to their professional services by auxiliary personnel. Under the new definition, CMS believes services provided incident to the professional services of an eligible distant site physician or practitioner could be reported when they meet direct supervision requirements at both the originating and distant site through the virtual presence of the billing physician or practitioner.
The duration of this change is time-limited because CMS has concerns that widespread direct supervision through virtual presence may not be safe for some clinical situations. For instance, virtual direct supervision might not be appropriate in complex, high-risk, surgical, interventional, or endoscopic procedures, or for patients with dementia, or patients where an in-person physical examination is necessary and important. CMS is seeking comments as to whether there should be any additional “guardrails” or limitations to ensure patient safety/clinical appropriateness, beyond typical clinical standards, as well as restrictions to prevent fraud or inappropriate use if this new definition were to become permanent beyond December 31, 2021. CMS also seeks information on what risks this policy might introduce to beneficiaries as they receive care from practitioners that would supervise care virtually in this way. Commenters are invited to provide data and information about their implementation experience with direct supervision using virtual presence during the PHE, including comments on the degree of aging and disability competency training that is required for effective use of audio/video real-time communications technology.
CMS proposed changing the frequency limitation to cover subsequent nursing facility care services furnished via telehealth to once every 3 days (the current rule covers it only once every 30 days). The original 30 day restriction was due to concerns on the acuity and complexity of nursing facility residents, and to ensure nursing facility residents have frequent encounters with their admitting practitioner. However, CMS has been persuaded that the use of telehealth is crucial to maintaining a continuum of care in nursing facilities, and to honor the independent medical judgment of treating clinicians to decide whether telehealth vs in-person care should be used depending on the needs of each specific resident.
CMS did not propose changing the frequency limitations for subsequent inpatient hospital telehealth services (once every 3 days). But CMS is seeking comments if it would enhance patient access to care if frequency limitations were removed altogether (and, if so, how best to ensure that patients receive in-person care when necessary).
To facilitate billing of CTBS by therapists, CMS proposed to designate HCPCS codes G20X0, G20X2, G2061, G2062, and G2063 as “sometimes therapy” services. When billed by a private practice PT, OT, or SLP, the codes would need to include the corresponding GO, GP, or GN therapy modifier to signify that the CTB are furnished as therapy services furnished under an OT, PT, or SLP plan of care.
CMS received several requests to add new telehealth services. After review of the submissions, CMS proposed adding nine new codes to the list, set forth in the table below.
| Service Type | HCPCS Code | Service Descriptor |
| Visit Complexity Associated with Certain Office/Outpatient E/Ms | GPC1X | Visit complexity inherent to evaluation and management associated with primary medical care services that serve as the continuing focal point for all needed health care services (Add-on code, list separately in addition to an evaluation and management visit) |
| Prolonged Services | 99XXX | Prolonged office or other outpatient evaluation and management service(s) (beyond the
total time of the primary procedure which has been selected using total time), requiring total time with or without direct patient contact beyond the usual service, on the date of the primary service; each 15 minutes (List separately in addition to codes 99205, 99215 for office or other outpatient Evaluation and Management services) |
| Group Psychotherapy | 90853 | Group psychotherapy (other than of a multiple-family group) |
| Neurobehavioral Status Exam | 96121 | Neurobehavioral status exam (clinical assessment of thinking, reasoning and judgment, [eg, acquired knowledge, attention, language, memory, planning and problem solving, and visual spatial abilities]), by physician or other qualified health care professional, both face-to-face time with the patient and time interpreting test results and preparing the report; each additional hour (List separately in addition to code for primary procedure) |
| Care Planning for Patients with Cognitive Impairment | 99483 | Assessment of and care planning for a patient with cognitive impairment, requiring an independent historian, in the office or other outpatient, home or domiciliary or rest home, with all of the following required elements: Cognition-focused evaluation including a pertinent history and examination; Medical decision making of moderate or high complexity; Functional assessment (eg, basic and instrumental activities of daily living), including decision-making capacity; Use of standardized instruments for staging of dementia (eg, functional assessment staging test [FAST], clinical dementia rating [CDR]); Medication reconciliation and review for high-risk medications; Evaluation for neuropsychiatric and behavioral symptoms, including depression, including use of standardized screening instrument(s); Evaluation of safety (eg, home), including motor vehicle operation; Identification of caregiver(s), caregiver knowledge, caregiver needs, social supports, and the willingness of caregiver to take on caregiving tasks; Development, updating or revision, or review of an Advance Care Plan; Creation of a written care plan, including initial plans to address any neuropsychiatric symptoms, neuro-cognitive symptoms, functional limitations, and referral to community resources as needed (eg, rehabilitation services, adult day programs, support groups) shared with the patient and/or caregiver with initial education and support. Typically, 50 minutes are spent face-to-face with the patient and/or family or caregiver. |
| Domiciliary, Rest Home, or Custodial Care services | 99334 | Domiciliary or rest home visit for the evaluation and management of an established patient, which requires at least 2 of these 3 key components: A problem focused interval history; A problem focused examination; Straightforward medical decision making. Counseling and/or coordination of care with other physicians, other qualified health care professionals, or agencies are provided consistent with the nature of the problem(s) and the patient's and/or family's needs. Usually, the presenting problem(s) are self-limited or minor. Typically, 15 minutes are spent with the patient and/or family or caregiver. |
| 99335 | Domiciliary or rest home visit for the evaluation and management of an established patient, which requires at least 2 of these 3 key components: An expanded problem focused interval history; An expanded problem focused examination; Medical decision making of low complexity. Counseling and/or coordination of care with other physicians, other qualified health care professionals, or agencies are provided consistent with the nature of the problem(s) and the patient's and/or family's needs. Usually, the presenting problem(s) are of low to moderate severity. Typically, 25 minutes are spent with the patient and/or family or caregiver. | |
| Home Visits | 99347 | Home visit for the evaluation and management of an established patient, which requires at least 2 of these 3 key components: A problem focused interval history; A problem focused examination; Straightforward medical decision making. Counseling and/or coordination of care with other physicians, other qualified health care professionals, or agencies are provided consistent with the nature of the problem(s) and the patient's and/or family's needs. Usually, the presenting problem(s) are self-limited or minor. Typically, 15 minutes are spent face-to-face with the patient and/or family. |
| 99348 | Home visit for the evaluation and management of an established patient, which requires at least 2 of these 3 key components: An expanded problem focused interval history; An expanded problem focused examination; Medical decision making of low complexity. Counseling and/or coordination of care with other physicians, other qualified health care professionals, or agencies are provided consistent with the nature of the problem(s) and the patient's and/or family's needs. Usually, the presenting problem(s) are of low to moderate severity. Typically, 25 minutes are spent face-to-face with the patient and/or family. |
These nine services are sufficiently similar to services already on the list of Medicare telehealth services, so CMS classified them as Category 1 under a streamlined review process. Subject to public comment, these services are expected to be added to the list of Medicare telehealth services when the final rule is published, and would go into effect January 1, 2021. Note: for HCPCS 99437-99438, CMS the patient’s home can serve as a qualifying originating site when the patient is being treated for a substance use disorder or a co-occurring mental health disorder (in accordance with the SUPPORT Act).CMS rejected a request to add CPT 96040 (genetic counseling services) to the list. Genetic counselors are not allowed to bill Medicare directly for their professional services. Nor are genetic counselors eligible distant site practitioners for telehealth under the Social Security Act.
For 2021, CMS proposed creating a temporary Category 3 for those services added to the Medicare telehealth list during the public health emergency (PHE) for the COVID-19 pandemic that will remain on the list through the calendar year in which the PHE ends. CMS proposed adding thirteen codes to the list of Medicare telehealth services. We will discuss those Category 3 services, as well as the approximately 50 other codes CMS has temporarily added as telehealth services during the pendency of the PHE, in a companion article.
Providers, technology companies, and entrepreneurs interested in telehealth should consider submitting comments to the proposed rule anonymously or otherwise – via electronic submission at this link. Alternatively, commenters may submit comments by mail to:
If submitting via mail, please be sure to allow time for comments to be received before the closing date. CMS is soliciting comments on the proposed rule until 5:00 p.m. through the end of September.
Continued expansions in Medicare reimbursement mean providers should make enhancements to telehealth programs now, both for the immediate cost savings and growing opportunities for revenue generation, to say nothing of clinical quality and patient satisfaction. Though providers should be mindful of any sunset provisions on these expansions and be prepared to adjust operations in accordance with those timelines. We will continue to monitor CMS for any rule changes or guidance that affect or improve telehealth opportunities.
 Connect with Virtual Gynecology
Connect with Virtual Gynecology For additional background information, you can learn about the basics of Medicare telehealth services and CMS’ annual review process here. And for more information regarding telehealth, telemedicine, or virtual care, then connect with the team at Virtual Gynecology. Together, we’ll make healthcare more accessible to those who need it most.
The journal, Female Pelvic Medicine & Reconstructive Surgery, published a study comparing video visits to in-person office visits for postoperative care. To read the study, click the link below!
Researchers at the University of California, San Francisco have been evaluating hundreds of pregnant women who tested positive for coronavirus, and the impact it has had on themselves and their babies during pregnancy. The study aims to better understand the correlation between pregnancy and coronavirus. They also want to evaluate a diverse population for a more thorough grasp of the findings. The study is open for women 14 years or older who have tested positive for coronavirus or are experiencing symptoms. In addition, it will examine the impact of the virus on African American and underprivileged women who are more susceptible due to a lack of health care.
As of May 15th, 2020 The Pregnancy Coronavirus Outcomes Registry, or PRIORITY, has registered 706 women to participate in the study. The year long evaluation includes how the virus impacts maternal health, fetal development, early delivery, newborn health, transmission between mother and child, and the correlation between underprivileged women and the risk of higher mortality. Participants are asked to answer questions about their health and pregnancy, permission to review their medical records related to their coronavirus diagnosis and treatment, and contacted up to 7 times within the next year for routine checkups. The PRIORITY website states that they will continuously update their data so all of the information is available to the public eye. For more information about PRIORITY, click here to navigate to their homepage, and click here if you’re a healthcare provider who wants to refer someone, or if you are personally interested in joining the study.
Everyday Health released an article about the importance of making and keeping your appointment to see your gynecologist during the pandemic. If you are interested in learning more, click here to read the article! Make sure to book your appointment with our virtual gynecologist today.