Syphilis is primarily a sexually transmitted disease caused by the bacterium Treponema pallidum (because syphilis is in the genus Treponema, it can also be called a “treponemal disease”; however, there are other treponemal diseases that are not syphilis). It is transmitted through the mucous membranes, broken skin, and direct mother-to-child infection during pregnancy. As such, unprotected sex (anal, oral, vaginal, or any other permutation that results in the exchange of bodily fluids) increases an individual's risk of contracting the disease. Similarly, risky sexual behavior and increased number of sexual partners also increase an individual’s risk of contracting syphilis (and other sexually transmitted diseases).
Syphilis typically presents in three distinct symptomatic stages, (described below) marked by potentially long periods of symptom-free remission between stages. If left untreated, the final stage is usually ultimately fatal. However, it can take up to several decades from the point of initial infection until an individual enters the third and final phase of the disease.
As mentioned above, syphilis commonly presents with three distinct symptomatic stages. These are commonly known as Primary, Secondary, and Tertiary syphilis. Each stage is marked by its own set of typical signs and symptoms of the underlying disease.
● Primary Syphilis usually presents as a single round, painless, firm lesion called a chancre. It usually appears around the genitals or anus, but can occur elsewhere on the body. It usually appears within three weeks of the time of the initial infection. Even if left untreated, the chancre will usually heal within three to ten days.
● Secondary Syphilis usually presents as a more diffuse non-itchy rash across the skin. One of the distinct features of secondary syphilis is that this rash often can involve both the palms of the hands and the soles of the feet. Even if left untreated, this phase will also usually resolve on its own.
● Tertiary Syphilis may occur multiple decades after the initial infection, if left untreated. It can cause diffuse damage throughout the individual’s body to multiple different organ systems, from bone to skin and so forth. However, what often ends up claiming the lives of the afflicted individuals is the damage done to their brain and cardiovascular system. If there is clinical suspicion of syphilis, the individual will still require additional laboratory testing to confirm the diagnosis.
Individuals infected with syphilis can still be accurately tested even if they do not have any active symptoms suggestive of syphilis. This is done by a combination of two blood tests:
1. A nontreponemal test, such as the Venereal Disease Research Laboratory (VDRL) or Rapid Plasma Reagin (RPR) test.
2. A treponemal test, such as the Treponema pallidum Passive Particle Agglutination assay (TP-PA), Enzyme Immunoassays (EIA), Chemiluminescence Immunoassays (CIA), or rapid treponemal assays.
A positive result for both the nontreponemal and treponemal tests is required for a diagnosis of syphilis. Additionally, if there is access to drainage or fluid from an open lesion, urinary discharge, or the tissue from a lesion, darkfield microscopy can be used to look for visual confirmation of the presence of Treponema pallidum (which appear as little white spirals under the microscope, hence their alternate classification as a “spirochete” bacteria).
As dismal and dire as untreated syphilis is, the good news is that syphilis is easily treatable and curable if caught before entering the tertiary syphilis stage of the disease. The mainstay of treatment is an injection of a long-acting form of penicillin called benzathine penicillin G. Because syphilis can be transmitted directly from mother to child during pregnancy, treatment with benzathine penicillin G is highly recommended for infected pregnant women to prevent congenital syphilis in the child. There is even evidence supporting additional treatment for pregnant women. However, because of the additional risks, this issue should be discussed with the woman’s obstetrician to decide on the best treatment plan and course of action.
Book Appointment Now Call For An Appointment
From a purely brass-tacks scientific perspective, syphilis is just the name given to a three-stage disease caused by the bacteria Treponema pallidum. It is essentially transmitted through mucous membranes or broken skin, which is why the overwhelming method of transmission is unprotected sexual contact and the risk goes up rapidly in proportion to riskier sexual practices and increased number of sexual partners. It is also worth noting that the sexual partners of people with a high number of sexual partners are also more likely to have an increased number of sexual partners themselves, thus compounding the increased risk of exposure to syphilis.
Syphilis can also be transmitted directly from an infected mother to her unborn child. The untreated disease usually progresses through three distinct stages, punctuated by periods of spontaneous remission (often mistaken for an actual resolution of the disease) in between. The first stage is usually a single, painless, firm lesion on the skin called a chancre (most commonly on the genitals or anus, but it can occur elsewhere). The second stage is usually a more disseminated rash across the skin, notable for its presence on the palms and soles of the feet. The third and final stage is usually characterized by diffuse systemic involvement, but most notably including severe damage to the central nervous system and cardiovascular system. This third and final stage may occur decades after the initial infection, and often results in the death of the individual.
The exact geographic origin of syphilis is still a widely debated subject. Some theories posit that it originated in the Americas and was brought back to Europe by Christopher Columbus’ crew. Others posit that it originated in Africa or the Old World. And others suggest that it was endemic globally. There is good evidence of treponemal disease (syphilis) in Native Americans prior to 1492, thus making the American origin plausible. However, there is also some evidence of treponemal disease in Europe prior to 1493 (when Columbus’ crew returned), although this evidence is not as strong and is disputed by many. There is also evidence that syphilis originated in either cattle or sheep and made a zoonotic transmission to humans. This, of course, raises the possibility of --to put it delicately-- let’s just say a rather unorthodox approach to “animal husbandry”. Although it is also plausible that the jump to humans could have happened through less disturbing means, such as butchering the carcasses of infected animals with broken skin.
Over the centuries, what we now call “syphilis” has gone by many names and has often been conflated and confused with other sexually transmitted diseases -- and even diseases such as leprosy and leishmaniasis. Our current name “syphilis” actually originated from a set of fictional novels written in 1530 by the Italian poet Girolamo Fracastoro called, “Syphilis sive Morbus Gallicus”. In these books, Fracastoro ascribes the origin of the disease to a curse placed on the people of ancient Greece because a shepherd named Syphilis refused to worship the god Apollo. As one might expect, there is rampant speculation about many prominent historical figures who are believed to have had syphilis, ranging from Leo Tolstoy and Friedrich Nietzsche, to Al Capone and Adolf Hitler.
The actual bacterium responsible for syphilis (Treponema pallidum) was not identified until 1905 by Fritz Schaudinn and Erich Hoffmann in Germany, and the first (moderately) effective treatment for syphilis did not come until 1910. It was an arsenic-based drug called arsphenamine and, while it was effective in the treatment of syphilis, it carried considerable downsides and adverse side effects -- as one would expect from a drug derived from arsenic! The real game changer for the successful treatment of syphilis came with the discovery of penicillin. Even though penicillin was discovered by Alexander Fleming in 1928, it was not mass produced and introduced to the American market until 1943.
While syphilis is a potentially fatal disease, the good news is that it can now be easily tested for and successfully treated with a single injection of long-acting penicillin. Recognizing the disease early is important and we will cover that in the next blog post.
Book Appointment Now Call For An Appointment
Both the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) have recently reported drastically increased rates of syphilis and, correspondingly, congenital syphilis recently. The WHO estimates that 7.1 million people globally acquired syphilis in 2020. The table below from the CDC shows a 78.9% increase in syphilis cases generally over the 5-year period from 2018 to 2022. Even more concerning, over that same 5- year period there was a 183.4% increase in congenital syphilis (that is, syphilis transmitted from an infected pregnant woman to her unborn child), and a 937% increase from a decade ago.
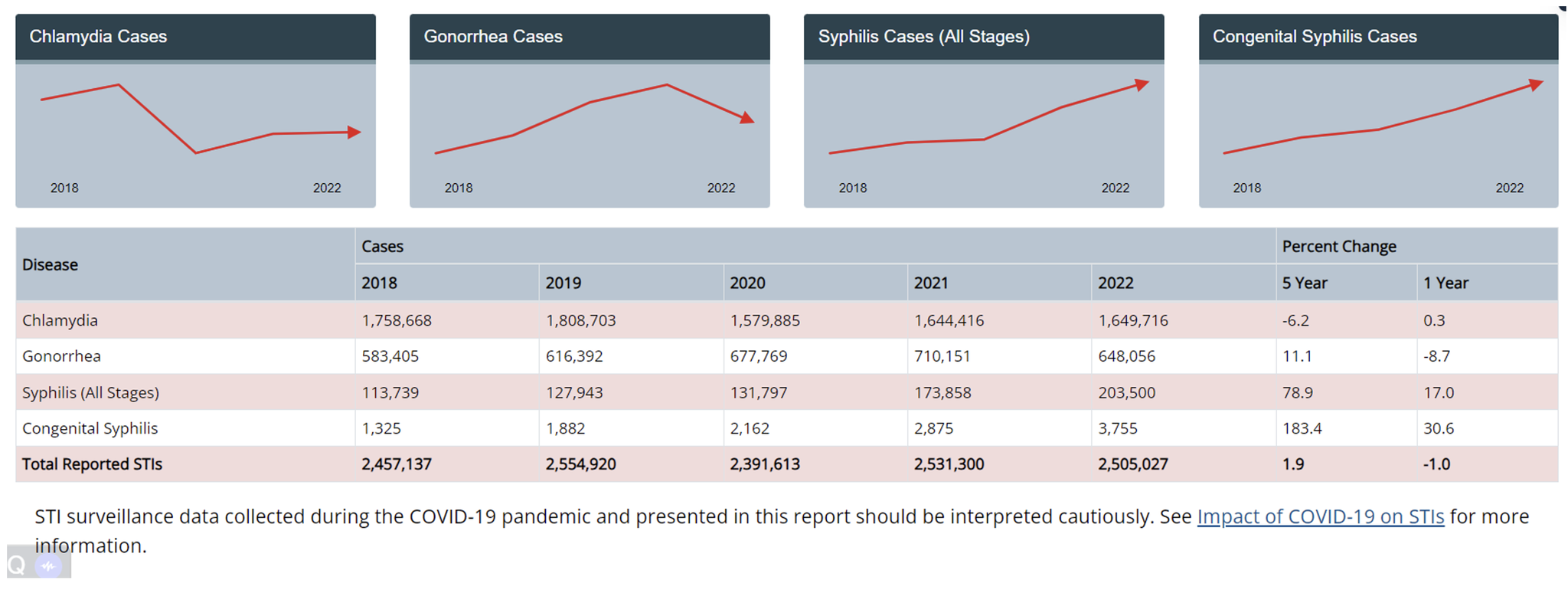
Among the greatest risk factors for syphilis are high risk sexual behaviors and a high number of sexual partners. However, what is surprising about the data is that the incidences of chlamydia and gonorrhea have remained relatively flat over that same 5-year time period. This would seem to suggest that there has not necessarily been an increase in risky sexual behaviors, but rather that the prevalence of syphilis has been increasing within the general population.
There are many potential reasons for this. One of the most commonly cited explanations by health organizations is insufficient testing for syphilis. One much less credible explanation given is a shortage of long-acting penicillin (trade name Bicillin) over the past year. While that might explain a rise over the past year, it does little to explain the rising trend over the 10 years prior. Moreover, there are other alternative treatments for syphilis, such as doxycycline.
One thing that is important to know about the disease course of syphilis is that it often has long periods where the infected individual may have no symptoms at all, and these periods can be up to decades long! Consequently, infected individuals who are asymptomatic are less likely to seek medical attention for testing and treatment. This, in turn, means that infected individuals could potentially be unwittingly transmitting the disease to others for years at a time before their syphilis symptoms recur and prompt seeking medical treatment. Syphilis is further complicated
by the fact that it can present in all manner of symptoms that one might not necessarily associate with a classic STD, thus leading to failure to successfully recognize and treat it. For this very reason syphilis is often colloquially called “the great imitator” amongst the medical community.
Greater awareness amongst both the general population and medical providers, combined with developing better and more frequent testing protocols would likely go a long way towards stemming the rising tide of syphilis. Successfully squelching syphilis need not be a Sisyphean task.
Book Appointment Now Call For An Appointment
When we think of sinusitis, common symptoms like nasal congestion, headaches, and facial pain come to mind. However, there's an uncommon symptom that often goes unnoticed - facial numbness. My Virtual Physician recognizes the importance of understanding this lesser-known connection and provides expert guidance on managing sinusitis effectively.
Sinusitis, an inflammation of the sinuses, typically brings discomfort around the nasal area. But can it cause numbness in the face? Indeed, in some cases, the inflammation and swelling can put pressure on facial nerves, leading to a sensation of numbness or tingling. This phenomenon is not widely known, and many may not immediately associate it with sinusitis. Understanding this link is crucial, as facial numbness can be alarming. It's a sign that sinusitis might be more severe or complicated than usual. My Virtual Physician emphasizes the importance of not dismissing such symptoms and seeking professional advice for a proper diagnosis.
Self-diagnosis can be risky, especially with symptoms like facial numbness. It's essential to consult healthcare professionals like those at My Virtual Physician. They can determine whether the numbness is indeed related to sinusitis or if it's a sign of another underlying condition. Sinusitis, especially when severe, can lead to complications if not treated appropriately. A professional diagnosis ensures that you receive the right treatment, preventing the condition from worsening or leading to further health issues.
In today's digital age, accessing healthcare has become more convenient through telemedicine services like My Virtual Physician. Consulting online for symptoms like facial numbness due to sinusitis not only saves time but also provides access to specialized care right from your home. My Virtual Physician offers comprehensive care for sinusitis, including understanding and managing unusual symptoms like facial numbness. Their expertise in telemedicine ensures that patients receive prompt and accurate diagnoses, followed by effective treatment plans.
If you're experiencing facial numbness along with other sinusitis symptoms, it's time to consult a physician. My Virtual Physician advises not to wait until symptoms become unbearable. Early consultation can lead to a quicker diagnosis and treatment, preventing the progression of the condition. Sinusitis with symptoms like facial numbness might require more than just over-the-counter medication. It's a sign that your body is reacting more intensely to the inflammation, and professional medical advice is crucial in such cases. Understanding Sinusitis in the Digital Age The rise of telemedicine has made managing health conditions like sinusitis more accessible. My Virtual Physician stands at the forefront, providing expert medical consultations online. For anyone experiencing sinusitis symptoms, especially something as unusual as facial numbness, My Virtual Physician offers a convenient and reliable solution. Remember, understanding your symptoms is the first step toward effective treatment. Don’t hesitate to reach out to My Virtual Physician for personalized advice and comprehensive care for your sinusitis concerns.
If you're experiencing symptoms of sinusitis, particularly facial numbness, consider booking an appointment with My Virtual Physician. Their team of experienced healthcare professionals is ready to provide you with personalized advice and comprehensive treatment options, all from the comfort of your home.
Sinusitis is more than just congestion and headaches. When it presents with a symptom like facial numbness, it's a sign to take action. My Virtual Physician is here to help you understand these symptoms and provide the care you need through convenient telemedicine services. Don't let sinusitis and its unusual symptoms go unchecked. Reach out to My Virtual Physician for expert care tailored to your needs.