Our previous post covered a brief introduction into what GLP-1 receptor agonist medications are. In this post we will expand a little further on the three main injectable GLP-1 medications on the market: liraglutide, semaglutide, and tirzepatide.
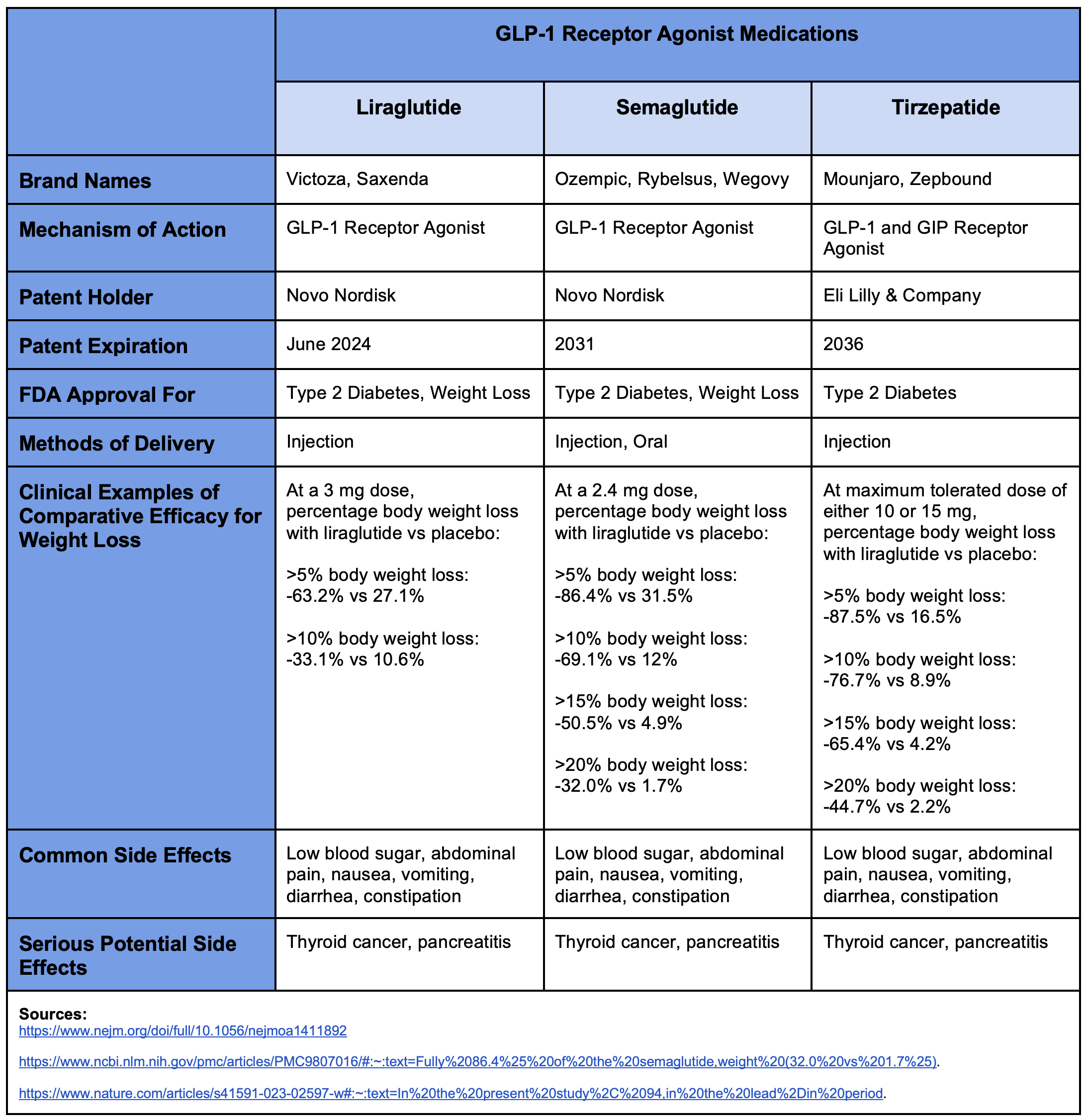
With regards to weight loss (as can be seen in the table), tirzepatide appears to perform the best of the three and liraglutide appears to be the least effective. For example, if we look at patients who successfully lost at least 10% of their body weight, we see that 76.7% of those on tirzepatide achieved this goal, 69.1% of those on semaglutide achieved it, and only 33.1% of those on liraglutide achieved it. The results for those in the placebo groups were all roughly comparable across all three drugs, thus suggesting that this is a roughly fair comparison. As one might expect, they all have fairly similar side effect profiles. And importantly of note, they all carry a potential risk of causing or exacerbating thyroid tumors. Consequently, patients with a personal or family history of thyroid cancer should make sure to discuss this with their physician before taking any of these medications.
In order to accurately consider the true cost-benefit ratio of medication you need to know the actual cost. Pricing for prescription medications is notoriously and deliberately obscure. The actual prices paid can vary enormously from state to state, from pharmacy to pharmacy, with different insurance companies, and even if you self-pay out of pocket. It can be surprisingly difficult to get a straightforward “universal price” for a prescription medication. The current “list prices” (like an MSRP) for liraglutide, semaglutide and tirzepatide are all roughly around $1,000 to $1,300 per month. And, as mentioned previously, there is not currently a generic version of any of the three GLP-1 receptor agonists we have been discussing. Consequently, while it is difficult to state the exact price at any given time, there currently is not a strong cost benefit to any of them versus the others.
However, as noted previously, liraglutide’s patent is set to expire in June of this year (2024). That means that we can reasonably expect a generic version to hit the market shortly thereafter. So, to answer the title question of whether or not there is a generic version of Ozempic, the answer is: “No, not quite yet in February 2024. But also yes, one of its major competitors should have a generic option later in 2024.” Once a generic option of liraglutide is on the market, its price will likely drop dramatically in short order. And as more generic manufacturers start producing liraglutide, the faster the price will decrease.
While it is regrettable that liraglutide seems to be the least effective of the GLP-1 medications for weight loss, it will also soon be the least expensive of them BY FAR -- and for the foreseeable future until semaglutide’s patent expires in 2031! Nevertheless, liraglutide is still undeniably an effective medication for weight loss and already has an FDA approval to be used as such. Furthermore, it is likely to cost a fraction of its competitors in late 2024. Consequently, it is highly probable that liraglutide will soon become the most cost effective medication for treating obesity within the not too distant future.
Chances are you've probably seen advertisements for drugs like Ozempic or Wegovy for weight loss. In fact, you probably even know someone who is taking one of them. So you may be wondering: what are they? Are they safe? And, perhaps more importantly, do they actually even work? Well, let’s get into it!
All these medications belong to a class of drugs called “GLP-1 receptor agonists” because they stimulate the Glucagon-Like Peptide-1 (GLP-1) receptor in the pancreas, which is a crucially important organ for regulating an individual’s blood sugar levels. Somewhat amusingly, these GLP-1 agonists were originally developed as a treatment for type 2 diabetes, since they stimulate an increase in insulin secretion (a hormone that lowers blood sugar) and a decrease in glucagon secretion (a hormone that counteracts insulin and raises blood sugar). However --and very serendipitously for the pharmaceutical companies-- it was subsequently discovered that one of the side effects of GLP-1 receptor agonists was weight loss! The pharmaceutical companies accidentally hit upon the proverbial jackpot.
Perhaps surprisingly, this type of accidental discovery happens all the time in pharmacology. A drug initially being developed for one purpose is found to have a “side effect” that may actually be more desirable than the original effect for which it was being developed. For example, sildenafil and minoxidil (better known by their brand names Viagra and Rogaine, respectively) both began their now-vaunted lives as failed blood pressure medications. So, too, with GLP-1 agonists.
While diabetes affects roughly 12% of the American population (certainly nothing to snub one’s nose at from a market opportunity perspective), the combined number of people who are either overweight or obese represent approximately 70+% of the American population -- and that is an almost irresistible siren call to the pharmaceutical companies to quickly repurpose those drugs as treatments for weight loss before the 20-year life of their patents expire!
In fact, the two brand name medications mentioned in the opening of this blog (Ozempic and Wegovy) are actually molecularly the exact same drug: semaglutide. It merely started being marketed to the general public as “Wegovy” once it received FDA approval to be sold as a weight loss drug versus an antidiabetic drug. Now, we must be clear: there is nothing necessarily wrong or untoward about marketing the same drug under a different brand name for treating different ailments (just check the variants of Excedrin!). One could even make the argument that it may be useful to help reduce potential confusion amongst consumers. Nevertheless, it is also useful for the informed consumer to know when the exact same thing is being marketed to them very differently under two different brand names intended to suggest the understanding that they are completely different products.
So, why even bring this up? The reason why it is important to understand this background information is because there are actually three prominent GLP-1 receptor agonist drugs currently on the market, and they all behave roughly in a similar manner: similar mechanism of action, similar effects, similar benefits, and similar undesirable side effects. These three drugs are liraglutide (name brands Victoza and Saxenda), semaglutide (name brands Ozempic, Rybelsus, and Wegovy), and tirzepatide (name brands Mounjaro and Zepbound). So far, only liraglutide and semaglutide have been approved by the FDA for weight loss, but tirzepatide’s FDA approval is likely only a matter of time. What’s notable at the present time is that liraglutide’s patent is set to expire in June of 2024, meaning that we can likely expect a much less expensive generic version to hit the market shortly thereafter.
Consequently, to be an informed consumer, it is worth considering how these three drugs stack up against each other to know which is the best optimization of costs to benefits. And, if one of them is about to considerably drop in price this year, how should that affect our decision matrix? So let’s compare these three GLP-1 receptor agonists!
People who have diabetes are twice as likely to have high blood pressure or ‘hypertension’ as those without diabetes. Hypertension occurs when there is an elevated pressure of blood pushing against blood vessel walls. Diabetes increases the risk of developing high blood pressure, at least in part, because excess sugar damages the small blood vessels, causing their walls to stiffen and thereby increasing the pressure of the blood pushing against the walls. Think of the blood vessels as rubber tubes, like hoses, that carry blood from the heart to the rest of the body. When the blood pressure is consistently high, it places strain on the arteries, causing damage which makes them less elastic and more prone to build up plaques. When these plaques form in the arteries in the heart they can become unstable and break off, causing a heart attack.
Both diabetes and hypertension increase the risk of heart disease, and that risk is additive (meaning the risk is higher if you have both diabetes and hypertension).
Heart disease is the #1 cause of death in the United States.
The standard way of measuring blood pressure in the hospital or doctor’s office is via a special device called a ‘sphygmomanometer’ which consists of an arm cuff that can be inflated with air to compress the artery and a meter that can measure pressure. The blood pressure is read as a ratio of two numbers, such as ‘130/80’. The top number is the systolic blood pressure, which measures the pressure of the blood in the arteries as the heart pushes blood out. The bottom number is the diastolic blood pressure, which measures the pressure of the blood in the arteries as the heart is resting and filling back up with blood. As you can imagine, systolic blood pressure will always be greater than diastolic blood pressure.
Treating high blood pressure, either with lifestyle changes like diet and exercise, medications, or a combination of the two, significantly reduces the risk of heart attacks and strokes. Large studies have shown that more intensive blood pressure control reduces the risk of heart disease, therefore the goal blood pressure is often lower for people with diabetes than those without. The most recent American Diabetes Association and World Health Organization guidelines, for example, both recommend considering a target blood pressure of < 130/80 for people with diabetes and hypertension.
Blood pressure goals vary, though, based on what is safe and practical for each individual. If you have hypertension and diabetes, it is best to talk with your health care provider to figure out the best approach.
Telemedicine provides a convenient way to get the care you need without traveling to the doctor or specialist you need. Virtual care, or Telehealth, has been around for a while, but recent changes in healthcare have caused telemedicine services to surge.
In the past, telemedicine visits were used primarily as urgent care encounters. If you had symptoms of a cold, you could chat with a Tel-a-doc and maybe get antibiotics.
Today, telemedicine services have expanded. And patients can see their telemedicine doctor for gynecologic, primary, and even wound care. In this post, we will look at how telemedicine has become a solution for patients with chronic or non-healing wounds by answering these questions.
Read on to learn more about telemedicine as a wound care solution.
Telemedicine is a healthcare delivery model that involves virtual consultations between patients and physicians, using online tools such as video conferencing, virtual examination rooms, and remote medical devices.
In many situations, telemedicine is ideal for individuals with wounds.
Those injured or struggling with chronic wounds may not feel like leaving home. Or they may be physically unable to leave home without assistance.
Often their caregivers work and cannot take time from work for frequent doctor appointments. Also, depending on where an individual lives, there may not be a wound specialist in the area. If there is a local certified wound care expert, they may have limited availability.
So, wound care appointments may be difficult to get.
Telemedicine providers with specialized training and certification in wound care can save patients and their families frequent trips to their doctor or wound clinic. Telemedicine for wound care is efficient. Doctors can conduct virtual visits, see the wounds, and make treatment recommendations through video.
Telemedicine also lets patients have virtual follow-up conversations with their doctors and send images when the wounds change.
Telemedicine decreases costs by reducing the need to travel long distances to the hospital or to consult with a physician. It improves the quality of life for patients with chronic wounds while maintaining high standards of wound care.
Since the COVID-19 pandemic, federal and state programs (Medicare and Medicaid) and private insurers have expanded coverage for telemedicine services, including wound care.
That is good news for patients with wounds who need to see a specialist. In many cases, your health insurance will cover the cost of your virtual visit and wound care supplies that your provider orders.
Your insurance may cover a virtual doctor visit for treatment if you have:
You can check with your insurance company to find out what they will cover or talk with a telemedicine provider and have them verify your insurance coverage before making an appointment.
Wound care specialists provide a variety of services through telemedicine. According to the Department of Health and Human Services, Telehealth services are especially helpful for monitoring and improving ongoing health issues, like chronic wounds.
A telemedicine wound care specialist can evaluate and treat wounds virtually by:
These services help patients get the right treatment to heal the wound quickly and return to normal lives.
Telemedicine specialists also coordinate your care with your other doctors or home health.
There are many advantages of using telemedicine wound care services, including:
It’s easy to see why telemedicine wound care services are growing.
While there are numerous benefits of telemedicine for patients, primary among them is the ease of convenience and the ability to access quality care fast. Wound care services provided through telemedicine are a great example of a wound care solution that is helping many individuals get the care they need.
If you have a skin wound that needs medical attention, talk with the My Virtual Physician team to find out if their telemedicine wound care services are right for you.
Contact us now for your low-cost appointment that your insurance may cover!
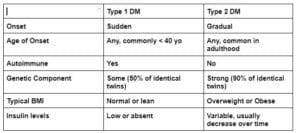
There are two main types of diabetes, type 1 and type 2. Formally, we refer to diabetes as diabetes mellitus (DM). The name is derived from the Greek word, diabetes, meaning to siphon or draw away liquid, and the Latin word, mellitus, meaning sweet. When diabetes was first recognized almost 700 years ago, it was described as a disease that caused people to urinate frequently and waste away. Frequent urination is still one of the first symptoms noted with new onset diabetes.
Usually, the sugar (glucose) in the blood is tightly regulated by a hormone called insulin. In people with diabetes, there is not enough insulin to push sugar into the cells, where it can be used for energy. As a result, the blood sugar becomes elevated and the kidneys have to filter an increased load of sugar out of the body via the urine. Although scientists didn’t have a laboratory test to check for sugar in the urine until the 1800s, tasting the urine for sweetness was a crude early method of diagnosis.
Although both type 1 and type 2 diabetes are defined by high blood sugar levels, the underlying cause of the high blood sugar is quite different. In type 1 diabetes, the insulin-producing beta cells in the pancreas are incorrectly identified as targets by the immune system. The immune system attacks the beta cells, the beta cells lose the ability to produce insulin, and the blood sugar becomes elevated. Because there is an absolute deficiency of insulin, people with type 1 diabetes require lifelong treatment with insulin.
In type 2 diabetes, on the other hand, there is not a single mechanism that has been identified as the underlying cause of elevated blood sugars. Rather, the cause is multifactorial, with both genetic and environmental factors contributing. The genetic component of type 2 diabetes is strong; almost 40% of individuals with type 2 diabetes have at least one parent with diabetes. Environmental factors, such as overweight/obesity, diets high in processed foods, and sedentary lifestyles have become increasingly prevalent in industrialized countries and have led to a steep rise in type 2 diabetes. Together, these genetic and environmental factors have been linked to the development of 1) impaired insulin secretion 2) resistance of the cells to insulin, and 3) ultimately type 2 diabetes. Usually, people with type 2 diabetes continue to secrete insulin for years, thus they can (at least initially) be treated with medications that work to either increase insulin from the pancreas or increase the cells’ ability to use the insulin already being produced.
Type 2 diabetes is the most common type of diabetes by far, accounting for 90-95 % of cases in the United States. It is estimated that about one out of every ten Americans has diabetes and, of those, 20% are unaware they have it.
If you are experiencing any symptoms of diabetes, such as frequent urination, blurry vision, numbness or tingling in your hands or feet, or unexplained weight loss, please check in with your health care provider to see if a diabetes screening test is indicated.